JOHNS HOPKINS
advertisement

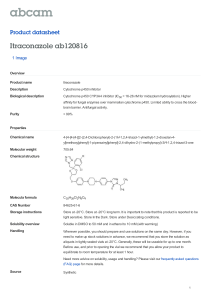
JOHNS HOPKINS U N I V E R S I T Y Department of Pathology 600 N. Wolfe Street / Baltimore MD 21287-7093 (410) 955-5077 / FAX (410) 614-8087 Division of Medical Microbiology THE JOHNS HOPKINS MICROBIOLOGY NEWSLETTER Vol. 25, No. 12 Tuesday, June 20, 2006 A. Provided by Sharon Wallace, Division of Outbreak Investigation, Maryland Department of Health and Mental Hygiene. 4 outbreaks were reported to DHMH during MMWR Week 23 (June 11-17, 2006): 3 Foodborne Gastroenteritis outbreaks 3 outbreaks of FOODBORNE GASTROENTERITIS associated with Restaurants (Frederick Co., & Montgomery Co.) and a Private Home (Queen Anne's Co.) 1 Gastroenteritis outbreak 1 outbreak of GASTROENTERITIS associated with a Daycare (Carroll Co.) B. The Johns Hopkins Hospital, Department of Pathology, Information provided by, Kathryn Johnson, M.D. Ph. D. Clinical presentation: The patient was a 62-year-old man with a history of lung cancer, status post lobectomy as well as relapsed mantle cell lymphoma status post nonmyeloablative bone marrow transplant and Cytoxan treatment. A few days after his BMT he began suffering from increasing night time temperatures. He also reported headache, nausea, vomiting and diarrhea. He did not complain of dyspnea or dysuria. He was admitted to JHH on 06/03/2006 for evaluation of neutropenia fever and diarrhea. Blood cultures were sent. He continued to deteriorate. Caspofungin and voriconazole were begun after the blood cultures grew Scedosporium prolificans. In total, he had seven positive blood cultures drawn over five days and two positive endotracheal cultures collected on the same day. He continued to rapidly deteriorate with multisystem organ failure and died on 06/07/2006. Organism,: Scedosporium prolificans (formerly known as Scedosporium inflatum) is a hyaline mold that typically produces an olive-gray to black, flat, silky colony surface on which water droplets tend to accumulate. The reverse surface often exhibits dark pigmentation. Microscopic examination reveals hyaline, septate hyphae with conidiogenic cells which may arise directly from hyphae or at the tips of the conidiophores, which are unbranched and flask-shaped with swollen bases and apical annellations. The conidia are brown, ovoid, smooth, thin-walled and measure 2-5 x 3-13 µm. The tips of the conidiogenic cells develop clumps of conidia. Detached conidia may also aggregate in clusters. Clinical significanceError! Bookmark not defined.,Error! Bookmark not defined.,: The epidemiology of Scedosporium prolificans has changed over the past 15 years. Before 1990, most cases of Scedosporium were from subcutaneous lesions or osteomyelitis/septic arthritis following trauma. Since 1990, septic arthritis or osteomyelitis following trauma to joints is still the most common clinical scenario; however, disseminated disease has been increasingly reported. These cases are primarily of immunosuppressed patients, especially those with prolonged neutropenia and post-transplantation therapy. Scedosporium prolificans is now recognized as the most common cause of disseminated phaeohyphomycosis. Colonization of the external ear, paranasal sinuses and lung, including "fungus ball" have been reported, as well as mycotic keratitis. An important aspect of this organism is its frequent resistance to antifungal therapy. Treatment: Scedosporium prolificans is resistant to amphotericin B, flucytosine, ketoconazole, miconazole, fluconazole and itraconazole, voriconazole and caspofungin. While itraconazole or terbinafine alone are not effective against most Scedosporium prolificans isolates, synergistic interactions were found in vitro between terbinafine and three azoles (voriconazole, miconazole, and itraconazole) against five clinical S. prolificans isolates. Due to its primary multi-resistant nature, treatment of Scedosporium prolificans infections is difficult and mortality unfortunately remains very high in most of the cases 1 Koneman, EW, et al. Color Atlas and Textbook of Diagnostic Microbiology, 6th edition. 2006 Sutton, DA; Fothergill, AW; and Rinaldi, MG. Guide to Clinically Significant Fungi. 1998. 3 Mycology Online: Scedosporium prolificans, © 2005 The University of Adelaide Last Modified 11/02/2005 David Ellis, CRICOS Provider Number 00123M. http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Hyphomycetes_(hyaline)/Scedosporium/prolificans.html 4 Revankar, S. G., J. E. Patterson, D. A. Sutton, R. Pullen, and M. G. Rinaldi. 2002. Disseminated phaeohyphomycosis: Review of an emerging mycosis. Clin Infect Dis. 34:467-476. 5 Doctorfungus, Scedosporium spp. http://www.doctorfungus.org/thefungi/Scedosporium.htm 6 Meletiadis, J., J. W. Mouton, J. L. Rodriguez-Tudela, J. Meis, and P. E. Verweij. 2000. In vitro interaction of terbinafine with itraconazole against clinical isolates of Scedosporium prolificans. Antimicrob. Agents Chemother. 44:470-472. 2