Application of PRINT® Microparticle and Nanoparticle Technology
advertisement

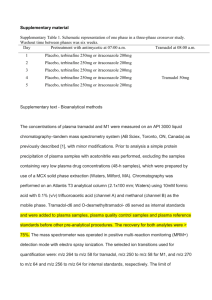
Application of PRINT Microparticle and Nanoparticle Technology – Toward Preparation of Ophthalmic Suspension Formulations with Improved Tolerability and Efficacy Benjamin Maynor, Andres Garcia, Janet Tully, and Benjamin Yerxa Liquidia Technologies, P.O. Box 110085, RTP, NC 27709 Corresponding Author: Benjamin Maynor, ben.maynor@liquidia.com, (919) 328-4354 Abstract Purpose: To use PRINT technology, a novel particle engineering approach, to produce micro and nanoparticles of controlled microstructure and nanostructure that are suitable for the preparation of aqueous ophthalmic suspension formulations without use of solubilizing excipients (e.g. cremaphor, oils, cyclodextrins). Platform Capabilites for “Hard to Formulate” Small Molecules and Biologics Dissolution Testing of Itraconazole Particles The dissolution protocol and medium was optimized in order to ensure maintenance of sink conditions throughout the course of dissolution testing. Dissolution medium consisted of 0.1N HCl, and 0.3% SDS at pH 1.2, consistent with previously published work (1). In addition, PVOH was used as a dispersing agent, which did not affect solubility at the concentrations tested. Based on these data, samples were tested at 10 µg/mL, a level sufficiently below the solubility limit of itraconazole. Methods: PRINT technology, a novel drug/excipient micromolding approach, was used to produce monodisperse nonspherical particles of itraconazole, cyclosporine, and tacrolimus. Dissolution characteristics of itraconazole suspensions were evaluated and compared to bulk and micronized itraconazole using standard dissolution test methods. Cyclosporine Results: Monodisperse, shape-specific microparticles and nanoparticles were successfully prepared of cyclosporine, tacrolimus, and itraconazole. Characterization of these particles using scanning electron microscopy confirms that monodisperse populations of particles were produced of cyclosporine, tacrolimus, and itraconazole, respectively. The sizes and shapes of these microparticles and nanoparticles are suitable for use in ophthalmic suspension dosage forms. Dissolution studies of itraconazole cylinder suspensions indicate that these particles dissolve faster under sink conditions than traditional micronized itraconazole (50% dissolution at 5 min for PRINT-itraconazole cylinders vs. 15 minutes for micronized itraconazole), suggesting that itraconazole PRINT formulations may have greater ocular surface bioavailability than traditional micronized formulations. Tacrolimus PRINT-Itraconazole has Increased Dissolution Rate Polymer nanoparticles Monoclonal Antibody Minimal Aggregation/Degradation of “Delicate” Actives PRINT® Technology • Brings the precision and control of semiconductors to life sciences and other markets • Proprietary design and manufacturing platform to produce nanoparticles and films • Monodisperse feature morphology designed into master template • Readily scalable using proven roll -to-roll manufacturing process Active Ingredient Relative Purity Steroids (various) > 99% Prostaglandins (various) > 98-99% Monoclonal Antibodies (bevacizumab, others) > 90-100 % siRNA > 99% Enzymes/proteins > 99% PRINT-itraconazole particles display faster dissolution than jet milled and bulk itraconazole, as evidenced by the time required to achieve 50% dissolution. This time was l5 min, 10 min, 20 min, and 45 min for the PRINT cylinders, jet milled-F1, jet milled-F2, and bulk itraconazole preparations respectively. Example: Itraconazole Microparticles Scanning Electron Micrographs (SEM) of particles generated from pure itraconazole. Top, left panel: 1 µm PRINT cylinders* Top, right panel: Jet milled powder (F1)* PRINT Process. A precise mold having micro- or nanoscale cavities (upper middle) is then filled with drug product and formed into particles (top row, right). Particles can be removed (bottom row, middle) from the mold and isolated as stable dispersions or free flowing powders (bottom row, left). 1 µm PRINT pollen 3 µm PRINT torus Bottom, left panel: 1 µm PRINT pollen; Bottom, right panel: 3 µm PRINT torus * Adapted from Garcia et al, 2012 (2) Benefits of the PRINT Platform for Ocular Drug Delivery 2 µm Implants Extended release formulations of biologics and small molecule drugs Reproducible implant size, dose and cost-effective manufacturing New targets for tissue delivery in the eye Simple delivery Micro/Nano Particles Topical delivery with fewer doses Sustained release Targeted drug delivery 2 µm PRINT Dexamethasone PLGA implants Particle type Particle Size (VMD) Jet milled itraconazole (F1) 3.63 µm3 Jet Milled itraconazole (F2) 2.52 µm3 PRINT hydrogel microparticles PRINT 1 µm cylinders 1.42 µm3 Summary of particle sizel characteristics for PRINT versus jet milled pure itraconazole measured by laser diffraction (VMD) and cascade impaction. These data demonstrate a reduction in volume median diameter (VMD), as well as an increased emitted dose (ED) and fine particle fraction (FPF), for the PRINT inhalation powder. Conclusions • • • Small molecules, biologics, and polymer microparticles and nanoparticles were formulated with high monodispersity and controlled geometry using PRINT technology PRINT process preserves biochemical activity and physical structure of API Enhanced dissolution kinetics were observed of microfabricated itraconazole particles, compared to traditional crystalline or micronized forms, which may enhance bioavailability of poorly soluble compounds Methods: • Itraconazole PRINT particles were fabricated using a proprietary molding process, as previously described (2). Jet milled itraconazole was prepared using a Glen Mills Laboratory Jet Mill. • Particle physical morphology was characterized by scanning electron microscopy. • Volume median diameter (VMD) was determined by laser diffraction. • The dissolution profiles were measured using an itraconazole suspension containing 0.1% w/w polyvinyl alcohol, acting as a wetting agent, and at a final drug concentration of 10 µg/ml. The dissolution medium consisted of 0.1N HCl and 0.3% w/w SDS and was maintained at a stirring speed of 100 RPM, as previously described for the evaluation of itraconazole formulations for pulmonary delivery (1). Sink conditions were maintained throughout. Dissolution test samples were removed and filtered using a 0.22 µm PES filter (Millipore) every 5 minutes for 30 minutes, then at 45, 60, 90, 120 and 240 minutes. Itraconazole content was measured using a RP-HPLC isocratic method and Waters Symmetry Shield RP18 column, 3.5 µm particle size, 4.6 x 150 mm analytical column. Mobile phase consisted of 20 mM hexanesulfonic acid and methanol (20:80) and a flow rate of 1mL/min was used. UV absorbance of itraconaozle, with a retention time of 4.5 minutes, was measured at 260 nm. Conflict of Interest B. Yerxa, J. Tully, A. Garcia, and B. Maynor are alll employees and shareholders of Liquidia Technologies, References: 1. McConville et al. (2006), “Targeted High Lung Concentrations of Itraconazole Using Nebulized Dispersions in a Murine Model,” Pharmaceutical Research, 23(5), pp 901-911. 2. Garcia et al. (2012), “Microfabricated engineered particle systems for respiratory drug delivery and other pharmaceutical applications,” Journal of Drug Delivery