File - Dr. Jerry Cronin
advertisement

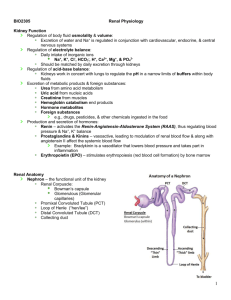
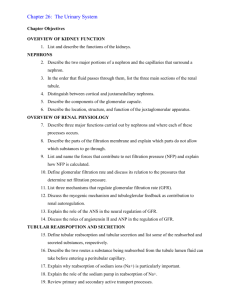
Glomerular Filtration Normally, 3 Starling forces are at work in glomerular filtration Glomerular Filtration • Regulation of the GFR is critical to maintaining homeostasis and is regulated by an assortment of local and systemic mechanisms: – Renal autoregulation occurs when the kidneys themselves regulate GFR. – Neural regulation occurs when the ANS regulates renal blood flow and GFR. – Hormonal regulation involves angiotensin II and atrial natriuretic peptide (ANP). Glomerular Filtration • Renal autoregulation of GFR occurs by two means: – Stretching in the glomerular capillaries triggers myogenic contraction of smooth muscle cells in afferent arterioles (reduces GFR). – Pressure and flow monitored in the macula densa provides tubuloglomerular feedback to the glomerulus, causing the afferent arterioles to constrict (decreasing blood flow and GFR) or dilate (increasing blood flow and GFR) appropriately. Glomerular Filtration • Neural regulation of GFR is possible because the renal blood vessels are supplied by sympathetic ANS fibers that release norepinephrine causing vasoconstriction. – Sympathetic input to the kidneys is most important with extreme drops of B.P. (as occurs with hemorrhage). Glomerular Filtration Two hormones contribute to regulation of GFR Angiotensin II is a potent vasoconstrictor of both afferent and efferent arterioles (reduces GFR). A sudden large increase in BP stretches the cardiac atria and releases atrial natriuretic peptide (ANP). • ANP causes the glomerulus to relax, increasing the surface area for filtration. The Filtration Membrane Podocyte of visceral layer of glomerular (Bowman’s) capsule Filtration slit Pedicel 1 Fenestration (pore) of glomerular endothelial cell: prevents filtration of blood cells but allows all components of blood plasma to pass through 2 Basal lamina of glomerulus: prevents filtration of larger proteins 3 Slit membrane between pedicels: prevents filtration of medium-sized proteins (a) Details of filtration membrane Pedicel of podocyte Filtration slit Basal lamina Lumen of glomerulus Fenestration (pore) of glomerular endothelial cell (b) Filtration membrane TEM 78,000x Glomerular Filtration (Interactions Animation) Renal Filtration You must be connected to the internet to run this animation Pressures That Drive Glomerular Filtration 1 GLOMERULAR BLOOD HYDROSTATIC PRESSURE (GBHP) = 55 mmHg 2 CAPSULAR HYDROSTATIC PRESSURE (CHP) = 15 mmHg 3 BLOOD COLLOID OSMOTIC PRESSURE (BCOP) = 30 mmHg Afferent arteriole Proximal convoluted tubule Efferent arteriole NET FILTRATION PRESSURE (NFP) =GBHP – CHP – BCOP = 55 mmHg 15 mmHg 30 mmHg = 10 mmHg Glomerular (Bowman's) Capsular capsule space Tubular Reabsorption • Tubular reabsorption is the process of returning important substances (“good stuff”) from the filtrate back into the renal interstitium, then into the renal blood vessels... and ultimately back into the body. Tubular Reabsorption The “good stuff” is glucose, electrolytes, vitamins, water, amino acids, and any small proteins that might have inadvertently escaped from the blood into the filtrate. Ninety nine percent of the glomerular filtrate is reabsorbed (most of it before the end of the PCT)! To appreciate the magnitude of tubular reabsorption, look once again at the table in the next slide and compare the amounts of substances that are filtered, reabsorbed, and excreted in urine. Tubular Reabsorption Amount in 180 L of filtrate (/day) Amount returned to blood/d (Reabsorbed) Amount in Urine (/day) 3L 180 L 178-179 L 1-2 L Protein (active) 200 g 2g 1.9 g 0.1 g Glucose (active) 3g 162 g 162 g 0g Urea (passive) 1g 54 g 24 g 30 g (about 1/2) (about 1/2) 0.03 g 1.6 g 0g 1.6 g (all filtered) (none reabsorbed) Total Amount in Plasma Water (passive) Creatinine Tubular Reabsorption • Reabsorption into the interstitium has two routes: – Paracellular reabsorption is a passive process that occurs between adjacent tubule cells (tight junctions do not completely seal off interstitial fluid from tubule fluid.) – Transcellular reabsorption is movement through an individual cell. Tubular Reabsorption • It is a tremendous feat to reabsorb all of the nutrients and fluid we must to survive, while still filtering out, concentrating and excreting toxic substance. – To accomplish this, the kidney establishes a countercurrent flow between the filtrate in the limbs of the Loops of Henle and the blood in the peritubular capillaries and Vasa Recta. • Two types of countercurrent mechanisms exist in the kidneys: countercurrent multiplication and countercurrent exchange. Tubular Reabsorption • Countercurrent multiplication is the process by which a progressively increasing osmotic gradient is formed in the interstitial fluid of the renal medulla as a result of countercurrent flow. • Countercurrent exchange is the process by which solutes and water are passively exchanged between the blood of the vasa recta and interstitial fluid of the renal medulla as a result of countercurrent flow. – This provides oxygen and nutrients to the renal medulla without washing out or diminishing the gradient. Tubular Reabsorption Both mechanisms contribute to reabsorption of fluid and electrolytes and the formation of concentrated urine. Tubular Reabsorption Reabsorption of fluids, ions, and other substances occurs by active and passive means. A variety of symporters and antiporters actively transport Na+ , Cl– , Ca2+, H+, HCO3– , glucose, HPO42– , SO42– , NH4+, urea, all amino acids, and lactic acid. Reabsorption of water can be obligatory or facultative, but it always moves by osmosis down its concentration gradient depending on the permeability of the tubule cells (which varies between the PCT, the different portions of the loop of Henle, DCT, and collecting ducts). Tubular Reabsorption • Obligatory reabsorption of water occurs when it is obliged to follow the solutes as they are reabsorbed (to maintain the osmotic gradient). • Facultative reabsorption describes variable water reabsorption, adapted to specific needs. – It is regulated by the effects of ADH and aldosterone on the principal cells of the renal tubules and collecting ducts. Tubular Reabsorption • This graphic depicts the formation of a dilute urine, mostly through obligatory reabsorption of water. • Compare this process to the one depicted on the next slide where urine is concentrated by the action of ADH on the DCT and collecting ducts of juxtamedullary nephrons.