1 - De Anza College
advertisement
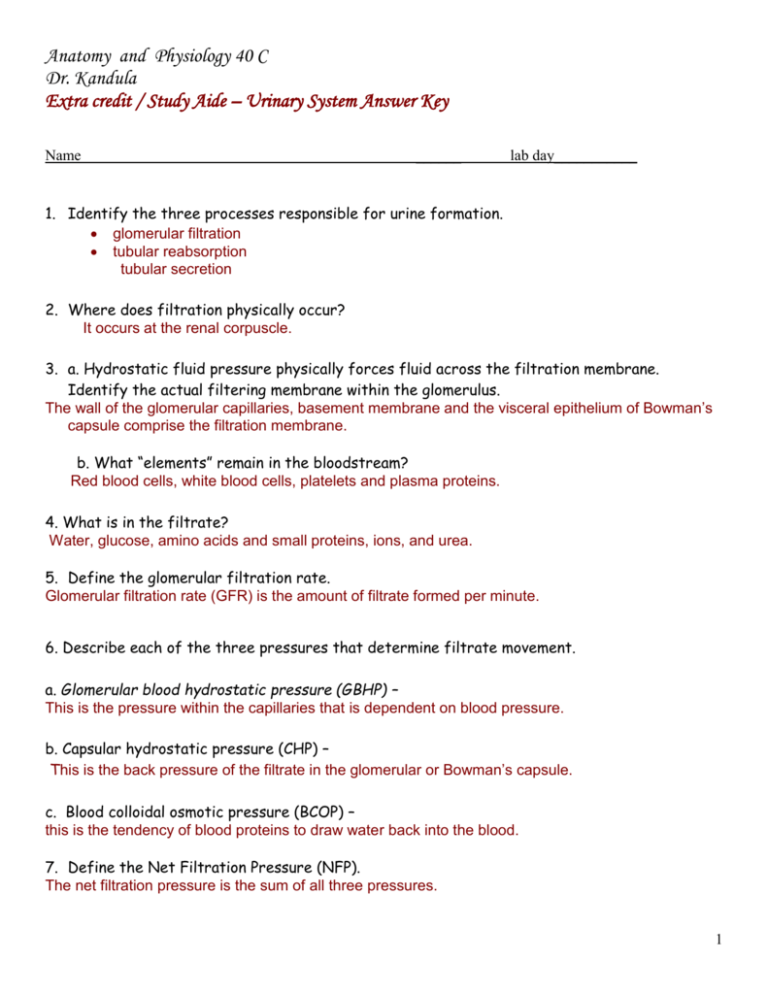
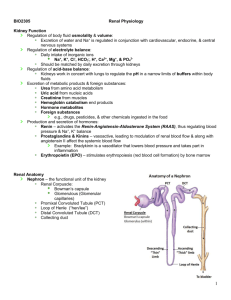
Anatomy and Physiology 40 C Dr. Kandula Extra credit / Study Aide – Urinary System Answer Key Name ______ lab day___________ 1. Identify the three processes responsible for urine formation. glomerular filtration tubular reabsorption tubular secretion 2. Where does filtration physically occur? It occurs at the renal corpuscle. 3. a. Hydrostatic fluid pressure physically forces fluid across the filtration membrane. Identify the actual filtering membrane within the glomerulus. The wall of the glomerular capillaries, basement membrane and the visceral epithelium of Bowman’s capsule comprise the filtration membrane. b. What “elements” remain in the bloodstream? Red blood cells, white blood cells, platelets and plasma proteins. 4. What is in the filtrate? Water, glucose, amino acids and small proteins, ions, and urea. 5. Define the glomerular filtration rate. Glomerular filtration rate (GFR) is the amount of filtrate formed per minute. 6. Describe each of the three pressures that determine filtrate movement. a. Glomerular blood hydrostatic pressure (GBHP) – This is the pressure within the capillaries that is dependent on blood pressure. b. Capsular hydrostatic pressure (CHP) – This is the back pressure of the filtrate in the glomerular or Bowman’s capsule. c. Blood colloidal osmotic pressure (BCOP) – this is the tendency of blood proteins to draw water back into the blood. 7. Define the Net Filtration Pressure (NFP). The net filtration pressure is the sum of all three pressures. 1 8. a. Describe the consequences if glomerular pressure is too high. Filtration rate increases forcing more filtrate into the glomerular capsule and decreasing volume within the blood. b. Describe the consequences if glomerular pressure is too low. Filtration rate decreases forcing less filtrate into the glomerular capsule and increasing volume within the blood. 9. a. What is renal autoregulation Renal autoregulation occurs when the kidneys themselves regulate blood flow b. Two autoregulatory mechanisms maintain normal GFR. Describe how each of them can increase or decrease GFR. i. myogenic mechanism myogenic mechanism – As systemic BP goes up, the smooth muscle cells in the afferent arterioles stretch. The smooth muscle fibers of the afferent arterioles respond to stretching by contracting and reducing the blood flow to the glomerular capillaries. GFR decreases. ii. tubuloglomerular feedback – When blood pressure is above normal, rapid filtrate flow reduces ion retention so filtrate has more sodium, chloride and water. It is believed that vasoconstricting chemicals from the juxtaglomerular cells are released when the macular densa detects higher water and ion levels in the tubule. These chemicals cause vasoconstriction of the afferent arteriole reducing blood flow to the capillaries and GFR decreases. 10. a. Compare sympathetic stimulation with autoregulation of glomerular filtration while at rest. At rest, sympathetic stimulation is weak and renal autoregulation is the dominant mechanism for controlling GFR. b. When is sympathetic stimulation of glomerular filtration important? It is important during extreme rises or falls in blood pressure. 2 11. Describe sympathetic stimulation affects on the following with an extreme drop in blood pressure. a. afferent arterioles - the afferent arterioles vasoconstrict. b. juxtaglomerular cells - these cells secrete renin that will promote the formation of angiotensin II, another vasoconstrictor. c. What is the net result of these two affects and how do they maintain homeostasis? The net result of increased sympathetic stimulation is a reduction in blood flow to the glomerular capillaries and a decrease in GFR. 12. With dropping blood pressure, the walls of the renal arterioles collapse causing the juxtaglomerular cells to produce rennin, which in turn stimulates angiotensin II secretion. What is the affect of angiotensin II? It is a vasoconstrictor to the afferent arterioles reducing blood flow to the glomerular capillaries. 13. With a sudden increase in blood pressure, the heart atria secrete ANP. What is its affect on glomerular filtration? ANP is released into the blood stream and causes the mesangial cells of the glomerulus to relax, increasing the surface area of the capillaries. This increases the filtering area and increases GFR. 14.Where does renal absorption and secretion occur? Along the nephron tubule. 15. Define what happens during these processes. a. absorption - returns materials to the bloodstream thereby conserving those materials. b. secretion - moves materials from the blood stream into the tubule for eventual disposal. 16. Due to very high glomerular filtration rates, nearly the entire volume of the blood enters the renal tubules every 30 minutes. Obviously, most of it must be reabsorbed to avoid dehydration. a. What part of the tubule achieves most of the reabsorption? In the proximal convoluted tubule. b. Where does further reabsorption and “fine tuning” occur? In the rest of the nephron. 3 17. a. Describe paracellular reabsorption. Paracellular reabsorption is the mechanism where substances diffuse between cells. b. Describe transcellular reabsorption. Transcellular reabsorption is the mechanism whereby the substances pass through the cell. c.What kind of transport mechanisms are used for reabsorption? Either passive or active transport mechanisms are used. 18.a. Identify two reasons that make secretion important. Secretion of hydrogen ions help regulate pH Secretion of other substances eliminates them from the body. b. What kind of transport mechanisms are used for secretion? Secretion mechanisms only use active transport. 19. a. Describe the role of primary active transport with regard to sodium ions Na+. The major role of primary active transport is to move sodium from the cytosol of the tubule cell into the surrounding interstitial fluid surrounding the capillary. b. Describe the role of primary active transport with regard to potassium (K+) and hydrogen (H+) ion movement. As a secondary function it provides the driving force to move potassium and hydrogen ions from the interstitial fluid to the filtrate. c. Why is Na+ movement important with regard to movement across the membrane? Because the movement of sodium ions via active transport is to generate an electrochemical gradient between the filtrate and the interstitial fluid. 4 20. The energy stored in the sodium ion electrochemical gradient is used to transport other molecules back toward the bloodstream (reabsorption). What nutrients are transported in this fashion? Glucose, amino acids and other solutes being recovered from the filtrate. 21. . What determines the direction of water movement? Water moves via osmosis following the direction of reabsorbed solutes 22. Describe reabsorption at the proximal convoluted tubule. The majority of reabsorption occurs here. Most of the filtrate is reabsorbed back into the blood stream restoring plasma concentrations of water, ions, urea and nutrients. 23. a. Describe reabsorption along the descending limb of the loop of Henle. The major function here is to reclaim more ions and water. The thin loop is permeable to water while the thick limb is impermeable to water. b. Describe reabsorption along the ascending limb of the loop of Henle. At the thick ascending limb, sodium and chloride are reabsorbed and at the thin descending limb water is reabsorbed via osmosis following the osmotic gradient produced by even more ion reabsorption. 24. Describe reabsorption along the distal convoluted tubule By the time the filtrate reaches the distal convoluted tubule, 80% of the water has been reabsorbed. Sodium and chloride ions are reabsorbed via secondary active transport using Na/Cl symporters. Water follows the sodium flow via osmosis. 25. Where does secretion occur? Proximal tubules and collecting duct. 26.a. Describe H+ and NH4+ ion secretion into the urine. Hydrogen ions are secreted into the filtrate by Na/H antiporters. Ammonia within the tubule cells can bind with the hydrogen ions to form NH4. The Na/H antiporters can also secrete these ions into the filtrate. b. What affect does removal of these ions have on blood pH? Removing these ions raises blood pH. 5 24. a. What solutes are secreted at the collecting duct? The solutes are potassium ions. b. Describe how potassium ions (K+) are secreted from the blood into the urine. Potassium ions are actively pumped using a Na/K pump into the cytosol of the principal cells lining the collecting duct. Potassium ions then diffuse down their concentration gradient into the filtrate. Removing these excess ions from the blood maintains electrolyte concentrations. 6