Colorectal Cancer
Henry Yao
HMO1, Royal Melbourne Hospital
Colorectal Cancer
• Epidemiology
– Most common internal cancer in Western Societies
– Second most common cancer death after lung cancer
– Lifetime risk
• 1 in 10 for men
• 1 in 14 for women
– Generally affect patients > 50 years (>90% of cases)
Colorectal Cancer
•
Forms
– Hereditary
• Family history, younger age of onset, specific gene defects
• E.g. Familial adenomatous polyposis (FAP), hereditary
nonpolyposis colorectal cancer (HNPCC or Lynch syndrome)
– Sporadic
• Absence of family history, older population, isolated lesion
– Familial
• Family history, higher risk of index case is young (<50years)
and the relative is close (1st degree)
•
Histopathology
– Generally adenocarcinoma
Risk Stratification
• Risk factors
– Past history of colorectal cancer, pre-existing adenoma,
ulcerative colitis, radiation
– Family history – 1st degree relative < 55 yo and relatives
with identified genetic predisposition (e.g. FAP, HNPCC,
Peutz-Jegher’s syndrome) = more risk
– Diet – carcinogenic foods
• Risk category (for asymptomatic pts)
– Category 1 (2x risk) – 1o or 2o relative with colorectal cancer
>55 yo
– Category 2 (3~6x) – 1o relative < 55yo or 2 of 1o or 2o
relative at any age
– Category 3 (1 in 2) – HNPCC, FAP, other mutations
identified
Screening
Group
Screening
Evidence
General Population
FOBT every 2 years from age 50 to 75
1A
Category 1
FOBT yearly +/- 5 yearly sigmoidoscopy
from age 50
Category 2
FOBT yearly + colonoscopy 5 yearly
from age 50 or 10 years younger than
index case
IIIB
Category 3
Variable Consult Oncology, e.g.
- FAP – colonoscopy every 12 months
from 12-15 yo until age 35 then 3 yearly
- HNPCC – 1~2yearly colonoscopy from
age 50 or 5 years younger than index
case
IIIB
Clinical Presentation
• Depends on location of cancer
• Locations
– ⅔ in descending colon and rectum
– ½ in sigmoid colon and rectum (i.e. within reach of
flexible sigmoidoscope)
• Caecal and right sided cancer
– Iron deficiency anaemia (most common)
– Distal ileum obstruction (late)
– Palpable mass (late)
Clinical Presentation
• Left sided and sigmoid carcinoma
– Change of bowel habit
• Alternating constipation + diarrhoea
• Tenesmus
• Thin stool
– PR bleeding, mucus
• Rectal carcinoma
– PR bleeding, mucus
– Change of bowel habits
– Anal, perineal, sacral pain
• Constitutional symptoms
– LOA, LOW, malaise
• Bowel obstruction
Clinical Presentation
• Local invasion
– Bladder symptoms
– Female genital tract symptoms
• Metastasis
– Liver (hepatic pain, jaundice)
– Lung (cough)
– Bone (leucoerythroblastic anaemia)
– Regional lymph nodes
– Peritoneum (Sister Marie Joseph nodule)
– Others
Examination
• Signs of primary cancer
– Abdominal tenderness and distension – large bowel
obstruction
– Intra-abdominal mass
– Digital rectal examination – most are in the lowest 12cm
and reached by examining finger
– Rigid sigmoidoscope
• Signs of metastasis and complications
– Signs of anaemia
– Hepatomegaly (mets)
– Monophonic wheeze
– Bone pain
Investigations
• Faecal occult blood
– Guaiac test (Hemoccult) – based on pseudoperoxidase
activity of haematin
• Sensitivity of 40-80%; Specificity of 98%
• Dietary restrictions – avoid red meat, melons, horseradish, vitamin C and NSAIDs for 3 days before test
– Immunochemical test (HemeSelect, Hemolex) – based on
antibodies to human haemoglobins
– Used for screening and NOT diagnosis
Investigations
• Colonoscopy
– Can visualize lesions < 5mm
– Small polyps can be removed or at a later stage by
endoscopic mucosal resection
– Performed under sedation
– Consent: bleeding, infection, perforation (1 in 3000), missed
diagnosis, failed procedure, anaesthetic/medical risks
– Warn: bowel prep, abdominal bloating/discomfort afterwards,
no driving for 24 hours
Bowel Prep
Investigations
• Double contrast barium enema
– Does not require sedation
– Avoids risk of perforation
– More limited in detecting small lesions
– All lesions need to be confirmed by colonoscopy and biopsy
– Performed with sigmoidoscopy
– Second line in patients who failed / cannot undergo
colonoscopy
Other Imaging
• CT colonoscopy
• Endorectal ultrasound
– Determine: depth, mesorectal lymph node involvements
– No bowel prep or sedation required
– Help choose between abdominoperineal resection or ultralow anterior resection
• CT and MRI – staging prior to treatment
• Blood tests
– FBE – anaemia
– Coagulation studies – for surgery
– UECr - ?take contrast, ?NAC required
– Tumour marker CEA
• Useful for monitoring progress but not specific for
diagnosis
Management
• Pre-operative
– Bowel prep – picolax, go lytely, fleet
• Normally 1 day prior
• Partial obstruction – 2~3 days prior
• Complete obstruction – intra-operative lavage
– Antibiotics prophylaxis (up to 24 hours post-op)
• Ampicillin
• Metronidazole
• Gentamicin
– DVT/PE prophylaxis
Arterial supply
Resection
Management
• Caecum or ascending colon
– Right hemicolectomy
– Vessels divided – ileocaecal and right colic
– Anastamosis between terminal ileum and transverse colon
• Transverse colon
– Close to hepatic flexure right hemicolectomy
– Mid-transverse extended right hemicolectomy (up to
descending) + omentum removed en-bloc with tumour
– Splenic flexure subtotal colectomy (up to sigmoid)
• Descending colon
– Left hemicolectomy
– Vessels divided – inferior mesenteric, left colic, sigmoid
Management
•
•
Sigmoid colon
– High anterior resection
– Vessels ligated – inferior mesenteric, left colic and sigmoid
– Anastomoses of mid-descending colon to upper rectum
Obstructing colon carcinoma
– Right and transverse colon – resection and primary anastomosis
– Left sided obstruction
• Hartmann’s procedure – proximal end colostomy (LIF) +
oversewing distal bowel + reversal in 4-6 months
• Primary anastamosis – subtotal colectomy (ileosigmoid or
ileorectal anastomosis)
• Intraoperative bowel prep with primary anastomosis (5% bowel
leak)
• Proximal diverting stoma then resection 2 weeks later
• Palliative stent
Rectal Cancer
• Options
– Low anterior resection
– Transanal local excision
– Abdomino-perineal resection
– Palliative procedure
• Factors influencing choice
– Level of lesion – distance from dentate line, <5cm requires
abdomino-perineal resection to obtain adequate margin
• Note: only 3% of tumours spread beyond 2cm
– Grade – poorly differentiated larger margin
– Patient factors – incotinence
– Mesorectal node status – resect if LN mets
Rectal Cancer
•
Anterior resection
– Upper and mid rectum cacinoma
– Sigmoid and rectum resected
– Vessels divided – inferior mesenteric and
left colic
– Mesorectum resected
– Coloanal anastomosis
– High – intraperitoneal anastamosis
(upper 1/3 of rectum)
– Low – extra-peritoneal anastomosis
– Post-op recovery
• Increased stool frequency
• 12-18 month to acquire normal bowel
function
• 1~4% anastamotic leak
Rectal Cancer
•
Abdominoperineal resection
– Larger T2 and T3 or poorly differentiated
tumour
– Rectum mobilised to pelvic floor through
abdominal incision
– Sigmoid end colostomy
– Separate perianal elliptical incision to
mobilise and deliver anus and distal
rectum
– Vessels ligated – inferior mesenteric
Rectal Cancer
• Hartmann’s procedure
– Acute obstruction
– Palliative
• Transanal local exision
– Early stage
– Too low to allow restorative surgery
• En block resection – for locally advanced colorectal carcinoma
(remove adherent viscera and abdominal wall)
• Palliative procedures
– Diverting stoma
– Radiotherapy
– Chemotherapy
– Local therapy – laser, electrocoagulation, cryosurgery
– Nerve block
Staging
•
•
TNM Staging
– Stage 0 – Tis N0 M0 – i.e. small tumour within the lining of the
colon or rectum
– Stage 1 – T1 N0 M0 or T2 N0 M0 – i.e. tumour has invaded layers
of the colon without spread beyond wall
– Stage 2 – T3 N0 M0 or T4 N0 M0 – i.e. tumour has spread beyond
wall and into nearby tissue but no LNs
– Stage 3 – Any T with any N but M0 – i.e. spread to nearby LNs but
not to other organs
– Stage 4 – Any T with any N and M1 – i.e. spread to other organs
(e.g. liver and lungs)
Duke’s staging
– Duke A – tumour confined to bowel wall
– Duke B – tumour invading through serosa
– Duke C – lymph node involvement
– Distant metastasis
Colon Cancer Summary
•
•
•
•
Wholistic care
– Education and counselling (about risk in family members as well)
– Lifestyle management – diet changes
– Support from cancer council
Surgical (hemicolectomy, stents for palliation)
– Stage 0 and 1 – surgical resection only with NO adjuvant chemo (NNT to high and SE
of chemo too high)
– Stage 2,3,4 – surgery, chemotherapy, radiotherapy, targeted therapy
– Prepare patient for surgery – explain diagnosis, surg under GA, hospital for 7d, bowel
prep, proph antibiotics, primary anastomosis, may require colostomy or ileostomy to
facilitate healing but temp and only for 12wk, risk is infection, bleeding, anastomotic
leak, mortality
Medical
– Adjuvant chemo – FOLFOX (folinic acid, 5-FU, oxaliplatin) – increase 5yr survival, be
wary of oxaliplatin causing peripheral neuropathy
– Biological therapy – anti-VEGF (bevacizumab), EGFR inhibitor (cetuximab)
– Radiotherapy – for palliation or liver mets
Follow-up
– Aim to detect local recurrence, metastasis or new primary
– CEA only useful if high b4 surg and low after surg
– FOBT, repeat CT, colonoscopy – according to hospital protocol
Rectal Cancer Summary
•
•
•
Wholistic care, conservative, (same colon cancer)
Medical and Surgical
– Neoadjuvant chemo-radiotherapy to reduce size and sterilize
area b4 surgery to reduce risk of recurrence
– Abdominal perineal resection (APR) → require permanent
colostomy as anus is removed
– Low anterior resection (LAR) – sphincter sparing surgery, upper
⅓ of rectum remove only and no stoma as anus is functional
– Local excision for superficial cancers
Follow-up
– Same as colon cancer
Complications
• Liver metastasis – resection, embolisation,
chemotherapy, RFA, cryotherapy
• Local invasion → perineal and pelvic pain
• Bowel obstruction
– Palliated surgically (colectomy, stoma, stent placed
endoscopically) or else syringe driver (mix of
analgesic, anti-emetic, anti-spasmotic)
• Fistula to skin or bladder
• Rectal discharge and bleeding
• Hypoproteinaemia (from poor appetite and absorption →
peripheral oedema)
• Poor appetite (steroids can help)
Prognosis
• 5 yr survivals
– T1 = >90%, T2 = >80%. T3 = >50%
– LN involvement = 30~40%
– Distant mets = <5%
Hereditary Colorectal Cancer
•
Familial adenomatous polyposis
– FAP account for <1% of all colorectal cancers
– Due to mutation of the adenomatosis polyposis coli (APC) gene
– Numerous adenomas appear as early as childhood and virtually
100% have colorectal cancer by age 50 if untreated
•
Hereditary non-polyposis colorectal cancer / Lynch syndrome
– More common than FAP and account for ~1-5% of all colonic
adenocarcinomas
– Due to a mutation in one of the mismatch repair genes
– Earlier age onset of colorectal cancer and predominantly involve
the right colon
– HNPCC also increases the risk of
• Endometrial, ovarian, breast ca
• Stomach, small bowel, hepatobiliary ca
– Renal pelvis or ureter ca
References
• Fry et al., Chapter 50 – Colon and Rectum, Sabiston Textbook
of Surgery 18th Edition
• Tjandra et al., Chapter 24 – Colorectal cancer and adenoma,
Textbook of Surgery 3rd Edition
• http://www.cancer.org.au//aboutcancer/cancertypes/colorectalca
ncer.htm
• Google images
Thanks You and Questions
© Copyright The University of Melbourne 2011
Case Scenario
• 70 year old male
• Presented to clinic
• “Doc, I have noticed some
blood in my stool.”
What are your differential diagnoses?
What do you want to ask on history?
Differential diagnosis
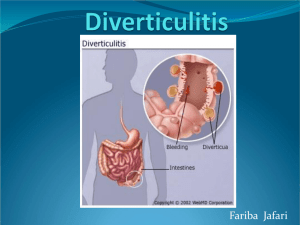
•
•
•
•
Common causes
– Haemorrhoids
– Colorectal cancer
– Diverticular disease
Anorectal pathology
– Haemorrhoids, anal fissure, anorectal cancer, anal prolapse
Colonic pathology
– Colorectal polyp/cancer, diverticular disease, angiodysplasia
– Colitis (IBD, infective, pseudomembranous colitis, ischaemic,
radiation)
– Post-surgery (e.g. polypectomy)
Small intestine and stomach pathology
– Massive upper GI bleed haematochezia
– Meckel’s diverticulum, small bowel angiodysplasia
History
• Seven characteristics of HOPC
• Key questions to sort out
– Age of onset
– Quality
• Insidious onset, mixed in with stool VS
• Intermittent, only with hard stools, blood on paper and
bowl and dabs of blood on top of stool
– Colour
• Black and tarry, associated with offensive smell
• Maroon red
• Bright red
• Torrential
– Past history of haemorrhoids, bowel cancer
– Family history of bowel cancer, breast cancer
Other history and examination
•
•
•
Other things to ask:
– Risk factors for haemorrhoids – constipation, heavy lifting, chronic
cough, pregnancy
– Other features of colorectal cancer
– Other features of colitis – pus and mucus in stool, fever, chills,
sweats
– Past medical history
Abdominal Examination
– Tenderness
– Masses
PR Examination
– Anorectal pathology
– Colour of blood on finger
– Polyps in rectum
Case Scenario
• Doc, I’ve been noticing
blood in my stool for 6
months now.
• The blood seems to be
mixed in the stool.
• I’ve also noticed some
constipation recently. This
is unusual for me. I
usually go every day.