Low Anterior Bowel Resection
advertisement

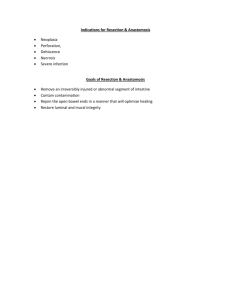
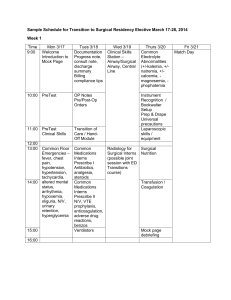
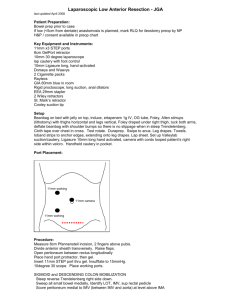
Clinical Scenario A 65-year-old obese male, former college biology professor, presents with 30 pound weight loss, fatigue, with inconstant occult bleeding and diarrhea of 4 months duration. He denies having any pain or tenesmus before, during or after urination and defecation. Patient’s 45-year-old sibling suffered from ulcerative colitis. Physical examination was unremarkable except for a guaiac positive stool. Differential Diagnosis Colorectal carcinoma Diverticulosis Familial Adenomatous Polyposis (FAP) syndrome Neoplastic polyps like tubular adenoma, villous adenoma Hyperplastic non-neoplastic polyps Required Tests Complete Blood Count (CBC) Flexible Sigmoidoscopy Colonoscopy Carcinoembryonic Antigen (CEA) test Immunochemical Fecal occult blood test (iFOBT) Digital rectal examination Fecal DNA test Double contrast barium enema and X-ray films Test Results Hematocrit 30%, hemoglobin 9.8 gm/dl. Chest X-ray was unremarkable. Sigmoidoscopy revealed a lesion 20 cm above the anus. CEA positive. Further evaluation shows no evidence of lymph node involvement or distant metastases. Differential Diagnosis Colorectal carcinoma Diverticulosis Familial Adenomatous Polyposis Tubular adenomas Hyperplastic polyps Colorectal Cancer Characteristics 3rd most common cancer and cause for cancer death in both males and females in the United States Highest incidence in high socioeconomic populations Etiology: dietary, hereditary, colorectal adenomas, ulcerative colitis Peaks in the 7th decade and localized mostly in the rectosigmoid colon Left side lesion: gross blood in stools, obstructive symptoms, encircling lesion Right side lesion: iron deficiency anemia, weakness, weight loss, right lower quadrant pain. Large sessile lesion Positive CEA is a reliable indicator of recurrent tumor Treatment Surgery procedure: Low Anterior bowel Resection (LAR). - Removing the diseased portion of the colon and rectum - En-bloc resection of mesentery and lymph nodes to reduce local recurrence - Anastomosing the remaining parts to create a functioning colon Technique: Hand-Assisted Laparoscopic Surgery (HALS) Chemotherapy and/or Radiation - Adjuvant therapy Patient and OR team position in HALS Patient is placed in a supine, 30 revered trendelenburg position and both legs are kept straight and slightly open to allow passage of the circular EEA stapler. The arm and hand of the left site of the planned resection are tugged by the patient's side. The surgeon initially stand on the left side of the patient for the sigmoidectomy and on the right side of the patient for the anterior resection and anastomosis. The surgeon assistant stands on the right side of the surgeon on either side of the patient. The scrub nurse and instrument table is positioned at the left lower extremity of the patient. Monitors are placed on both sides of the patient at the level of their shoulder. OR Set-up Surgical equipments Electronic CO2 laproflattor Laparoscopic suction irrigation machine Nasogastric tube and urinary catheter 5 mm and 10 mm trocars and cannula Gelport hand-access device 30- degree digital laparoscope connected to a fiber-optic cable machine Maryland dissector Harmonic scalpel Endo GIA universal stapling system. Electrosurgical knife EEA stapler Bowel grasper, scissors, rainer and spreader Incisions and trocar Midline umbilical incision (6-7 cm long) for placement of the Gelport hand-access device. Port is also used to insufflate the abdomen to 8 mmHg with CO2. Two 5 mm trocars were inserted on the left and right upper quadrant – used for non-traumatic bowel grasping, dissection and electrosurgical devices. A 10 mm trocar was placed infraumbilically – used for the digital laparoscope A12 mm trocar were placed on the right-lower quadrant – used for dissection, electrosurgical, clipping and stapling devices. Port Placement Surgical Procedure The dissection starts by medial to lateral dissection using the scissors, grasper and knife after pedicle ligation. The rectosigmoid and descending colon are mobilized by transecting the splenocolic ligament and the left colic branch of the inferior mesenteric artery with an electrosurgical cutter while preserving most of the mesentery to supply the anastomosis with the rectum. The colon is transected, with a GIA stapler, distal to the lesion at the planned site for the anastomosis The tumor –bearing segment is exteriorized through the hand Gelport site after application of a wound protector device and remove of the Gelport hand-access device. The diseased segment (colon and rectum) is resected extracorporeally with a GIA stapler The side of the stapler is secured with a purse-string around the distal colonic end, which is returned into the abdomen. The pneumoperitoneum is then established and the bowel end-to-end continuity is restored using a EEA stapling device through adequately irrigated rectal stump. All left-sided colonic and rectal anastomosis were carried out intracorporeally All left-sided anastomosis were tested for proper integrity. A drain was placed selectively if indicated and wounds were then closed in layers Post-operative care Patient allowed sips of water orally on the evening of the operation Free oral fluids are allowed on the first day, soft diet on the second day, and full diet and discharge on the thrid day Complications of HALS Wound infections Anastomotic breakdown leading to abscess or fistula formation and/or peritonitis Bleeding with or without hematoma formation Ischemic stricture, could be due to the stretch on the proximal colon during the extracorporeal anastomosis Incisional hernias at port site, from the continuous and persistent stretch or dehiscence (bursting of wound) Postoperative ileus Intraabdominal adhesions with minimal future risk of small bowel obstruction Benefits of HALS Restored tactile feedback Improves hand-eye coordination and allows safe finger dissection and retraction. Reduces hospital stays and rate of infections A mini-laparotomy hand Port incision. Reduced conversion rate in total laparoscopy. Enhanced safety and efficiency allowing the completion of the operation with a hand inside. Maintenance of the intra-abdominal pressure to facilitate the better view and magnification of laparoscopic telescope. Improving the steep learning curve for inexperienced general surgeons. Promising reduced cost-benefit ratio Limitations of HALS Fatigue of the surgeon since surgery last 4 hours on average Possible impaired tactile feedback through a lengthy complex procedure and Minor ergonomic restriction due to the crowdedness of the hand with the instruments. Not wells accepted by patient and surgeons because there is already a mini laparotomy. Cosmetically inferior than total laparoscopic surgery. References Vargas HD. Video on Low Anterior Bowel Resection using handassisted laparoscopic surgical technique. Department of Surgery, University of Kentucky. Ringley C, Lee YK, Igbal A, Bocharev V, Sasson A, McBride CL et all. Comparision of conventional laparoscopic and hand-assisted oncologic segmental colonic resection. Surg Endosc 2007; 21:2137-41 Meshikhes AN, Tair ME, Ghazal TA. Hand-assisted laparoscopic Colorectal Surgery: Initial Experience of a Single Surgeon. SJG 2011; 17:16-9 Cima R, Pemberton J. how a hand-assist can help in lap colectomy. Cont. Surg 2007; 63;1:19-23 Loungnarath R, Fleshman JW. Hand-assisted laparoscopic colectomy techniques Semin. Laparoscop Surg 2003; 10;4:219-230 QUESTIONS ?