Esophagus
advertisement

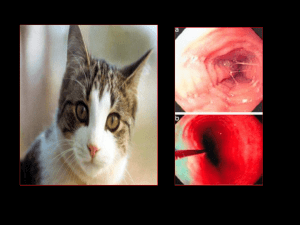
ESOPHAGUS anatomy physiology pathology treatment Anatomy of esophagus length 23-25 cm esophagus begins at the level of the sixth cervical vertebra and it enters into the superior mediastinum through the upper thoracic outlet then it descends into the posterior mediastinum and exits the thorax through esophageal hiatus of the diaphragm and enters the abdominal cavity there are three parts of the esophagus: cervical, thoracic and abdominal esophagus esophagus has three physiological constrictions Anatomy of esophagus It consists of three layers : arterial blood supply from: mucosa, submucosa muscular layer (circular and longitudinal layer) inferior thyroid artery descending aorta left gastric artery inferior phrenic artery venous drainage into the superior caval vein portal vein Anatomy of esophagus Esophagus has an extensive lymphatic drainage into cervical, posterior mediastinal, paraesophageal and celiac axis lymph nodes Anatomy of esophagus Carcinoma of the esophagus most common neoplasm of the esophagus is carcinoma its incidence is very differentiated worldwide and depends on geographical localization that proves its dependency on environmental factors 90% of patients with esophageal carcinoma die incidence of esophageal carcinoma is 8-12/100000 men per year in Europe and 6/100000 in the United States Carcinoma of the esophagus risk to develop carcinoma of the esophagus increases along with the age and is the highest between the sixth and the seventh decade of life more frequent in males main risk factors: smoking, alcohol incidence of esophageal adenocarcinoma raises Carcinoma of the esophagus Premalignant states Plummer-Vinson syndrome caustic burns achalasia Barrett’s esophagus leukoplakia Carcinoma of the esophagus Screening screening exfoliative cytology in endemic areas Barrett’s esophagus- endoscopic biopsy Carcinoma of the esophagus Clinical presentation dysphagia in 95% of cases regurgitation weight loss chest pain cough Carcinoma of the esophagus Diagnosis barium esophagogram flexible fiberoptic esophagoscopy with biopsy Computed Tomography endoscopic ultrasound – diagnostic accuracy 80– 90% Bronchoscopy Carcinoma of the esophagus Staging Primary tumor (size of tumor and depth of infiltration)–T regional lymph node involvement - N distal metastasis–M Carcinoma of the esophagus Staging Primary tumor - T T1 – tumor invades lamina propria or submucosa T2 – tumor invades muscularis propria T3 – tumor invades adventitia T4 - tumor invades adjacent structures Carcinoma of the esophagus Staging Regional lymph nodes – N N0 – no regional node metastasis N1 – regional node metastasis Distant metastasis – M M0 – no distant metastasis M1 – distal metastasis Carcinoma of the esophagus Surgical management radical – resection of a tumor with adequate oncological margins and regional lymph nodes palliative - to restore oral intake of food Carcinoma of the esophagus Most common surgical procedures 1. Thoracoabdominal Ivor–Lewis esophagectomy with high intrathoracic esophagogastric anastomosis and gastric drainage procedure 2. Thoracoabdominal McKeown esophagectomy with esophagogastric anastomosis in the neck 3. transhiatal Orringer esophagectomy with esophagogastric anastomosis in the neck 4. esophagectomy throuh left thoracophrenolaparotomy Carcinoma of the esophagus How to replace the esophagus? stomach- the best organ to replace the esophagus colon- the second organ for reconstruction small intestine (pedicle or free graft)- least appropriate Carcinoma of the esophagus Complications Postoperative complications from 20 to 40% perioperative mortality 3–10%, 20% was also reported Carcinoma of the esophagus Radiation therapy patients with advanced disease patients refusing to undergo surgery irradiation with a dose of 55–60 Gy usually used as a palliative treatment, unusually as a radical treatment has no influence on survival 5-year survival rate less than 6% Carcinoma of the esophagus Chemotherapy Effective for a short time recently advocated regimen is cisplatin with vindesine, bleomycin and 5-fluorouracil complete and partial response rates are reported for 25-50 % Carcinoma of the esophagus Combination therapy Results of monotherapy are bad 5-year survival rate after surgery alone is 10– 15 % most patients die due to distant metastases, hence local treatment is combined with systemic treatment Carcinoma of the esophagus Combination therapy - benefits decrease in tumor size early therapy for micrometastases enables the assessment of response to a used treatment and reassessment of staging after induction therapy surgery 3-6 weeks after induction therapy some authors question the role of surgery in improving survival Carcinoma of the esophagus Palliative therapy 50% of patients have distant metastases at the time of diagnosis main problem reported by a patient – dysphagia radiation therapy combined or not with chemotherapy offers immediate clinical improvement in dysphagia Carcinoma of the esophagus Palliative endoscopic treatment dilatation self-expanding stents stents laser ablation endoluminal brachytherapy photodynamic therapy Palliative resection, bypass procedures and gastrectomy are presently not advocated Self-expanding stents Carcinoma of the esophagus Prevention cessation of smoking and alcohol consumption treatment of Barrett’s esophagus detection of p53 gene mutation screening programs Rare esophageal malignancies Epithelial carcinoma planoepithelialae partim fusocellularae adenocarcinoma carcinoma basocellularae carcinoma microcellularae Non-epithelial leiomyosarcoma melanoma rhabdomyosarcoma fibrosarcoma Benign esophageal tumors Deriving from submucosa adenoma haemangioma papilloma fibrolipoma neurofibroma Deriving from muscular layer (intraparietal) leiomyoma lipoma fibroma Chemical burns of the esophagus Necrosis occurs directly after burn and is irreversible! Chemical burns of the esophagus Acids - they produce coagulative necrosis that is rarely full-thickness one. Similar injury should be expected in the stomach and duodenum. Caustic agents - they produce colliquative full-thickness necrosis including perforation. Classification of chemical burns of the esophagus I. Erythema, superficial exfoliation of esophageal epithelium shallow ulcerations not penetrating beyond submucosa, whitish discolorations II. A. superficial erosions and ulcerations B. deep, circumferential ulcerations III. deep ulcerations penetrating into the muscularis propria or producing perforation Chemical burns of the esophagus Clinical presentation a) severe retrosternal pain b) dysphagia c) shock d) respiratory disturbances e) subcutaneous emphysema in the necksometimes f) stridor and peritonitis- rarely Chemical burns of the esophagus First-aid treatment Oral administration of small amount of water administration of antidotes, advocated in the past, can trigger exothermic reaction and compound injury vomits shouldn’t be induced administration of antibiotics, steroids and analgesic agents. in a case of acute airway obstruction tracheostomy should be performed intravenous access Chemical burns of the esophagus First-aid treatment cessation of oral food intake chest x-ray examination esophagoscopy performed within 12-24 hours after burn preceded by laryngoscopy part of surgeons is of the opinion that endoscopy mustn’t be done and they advocate esophagogram using a water-soluble contrast medium if esophageal perforation is suspected, if not esophagoscopy can be done 2-3 days after burn and then 3 weeks after burn. Chemical burns of the esophagus Perforation of the esophagus occurs usually between 2 and 8 days after burn. Stricture of the esophagus after burn - treatment dilatation of stricture resection of the narrowed fragment of the esophagus and esophagoesophageal anastomosis- short strictures only esophagectomy and reconstruction using the stomach, colon or small bowel (possible malignant degeneration)- extensive esophageal strictures Thal or Collis gastroplasty- stenosis of gastroesophageal junction Perforation of the esophagus Esophageal perforation is a serious diagnostic problem. Incidence:1case per 8000 hospitalized patients per year and still increases due to growing number of diagnostic and therapeutic endoscopies. Perforation of the esophagus Etiology Iatrogenic from inside endoscopy dilatations variceral sclerosis esophageal intubation laser Perforation of the esophagus Etiology from outside mediastinoscopy intraoperative injuries (thyroid resection, enucleation of esophageal myoma, vagotomy, pneumonectomy) radiation therapy Traumatic blunt trauma penetrating trauma caustic injury Perforation of the esophagus Etiology Spontaneous perforation postemetic others e.g. childbirth Foreign body Neoplasms Paraesophageal infections Perforation of the esophagus Bacteria in saliva Infection Abscess, empyema , sepsis Air Emphyse ma Gastric juice Chemical burn Disturbances in Tension water and pneumothorax electrolyte balance shock mediastinum Perforation of the esophagus Clinical presentation Cervical esophagus neck ache increased on swallowing hemoptysis or hematemesis subcutaneous emphysema fever local tenderness change in the timbre of voice hydropneumothorax pneumothorax neck abscess Perforation of the esophagus Clinical presentation. Thoracic esophagus chest pain dyspnea subcutaneous emphysema pneumo- and hydrothorax tachycardia and tachypnea cyanosis fever Perforation of the esophagus Clinical presentation Abdominal esophagus peritonitis retrosternal pain radiating to the arms tachycardia and tachypnea fever Perforation of the esophagus Differential diagnosis Chronic gastric and duodenal ulcer disease myocardial infarction acute pancreatitis dissecting aortic aneurysm pneumonia pneumothorax Perforation of the esophagus Crucial aims of surgical treatment Elimination of sources of bacterial infection and chemical injury drainage of infected areas secure food intake Perforation of the esophagus Surgical management 1. 2. 3. 4. 5. primary repair of the perforation primary repair of the perforation buttressed with well-vascularized autologous tissue temporary exclusion of the perforated esophagus drainage procedures (T-tube drainage, washing drainage, intraesophageal drainage) partial or total esophageal resection Perforation of the esophagus Surgical management The earlier esophageal perforation is diagnosed the easier is a treatment. The later it is diagnosed the more aggressive should be a surgical management. Disorders of esophageal motility Disorders of esophageal motility can result both from its increased and decreased neuromotor activity . Cricopharyngeal achalasia Clinical presentation Cervical dysphagia Barium esophagogram demonstrates hypertonicity of the upper esophageal sphincter (narrowing of esophageal lumen) Presence of Zenker's diverticulum in some patients Treatment Cervical esophagomyotomy from the level of the superior cornu of the thyroid cartilage iferiorly to 1-2 cm behind the clavicle Neuromotor diturbances of esophageal motility Usually myotonic Observed in diseases such as: miasthenia gravis, dystrophia myotonica Pathologies of the peripheral and central nervous system. Diffuse esophageal spasm Clinical presentation Dysphagia, chest pain (retrosternal) Anxiety, signs and symptoms appear periodically x-ray examination and esophageal manometry demonstrate hypermotility Treatment Nitrates, calcium channel blockers Liquid, small-volume meals Long esophagomyotomy Achalasia Clinical presentation dysphagia regurgitation Lack of primary esophageal peristalsis, dilatation of the esophagus and the distal bird-beak taper of the esophagogastric junction on barium swallowing examination Luck of primary esophageal peristatlsis on manometry Achalasia Alteration of the central or peripheral vagal innervation. In many cases the lack or disintegration of ganglion cells in the myenteric (Auerbach's) plexus is observed. Etiology of achalasia is unknown. Achalasia Treatment Myorelaxants have weak or no therapeutic effect Dilatation of the lower esophageal sphincter Esophagomyotomy (Heller procedure) – 15% of cases Uchyłki przełyku Podział wrodzone nabyte prawdziwe rzekome Typ z uwypuklenia - uwypuklenia błony śluzowej i podśluzowej przez osłabiona mięśniówkę. Typ z pociągania - pociąganiu ściany od zewnątrz przełyku przez zapalnie lub bliznowato zmienione okołooskrzelowe i śródpiersiowe węzły chłonne. Diverticula of the esophagus Clinical presentation Dysphagia Regurgitation Bad breath Chest pain Typical roentgenographic picture Diverticula of the esophagus Complications Often asymptomatic clinical course Diverticulitis Fistula Abscess Bleeding Symptomatic patients or patients in whom complications occured should undergo surgical treatment.