Pediatric Laproscopic Nissen Fundoplication
advertisement

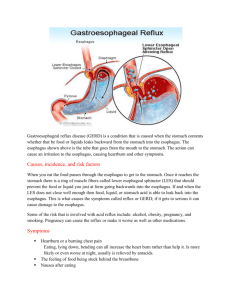
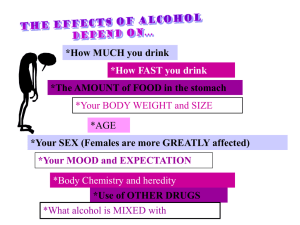
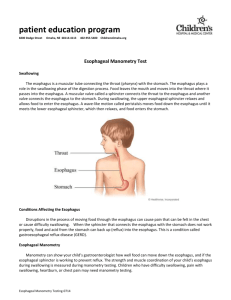
Pediatric Laproscopic Nissen Fundoplication Lindsey Bendure Minimally Invasive Surgery Lab Nissen Fundoplication The fundus of the stomach is wrapped around the esophagus so that the lower portion of the esophagus passes through a small tunnel of stomach muscle This strengthens the lower esophageal sphincter which prevents acid from retreating into the esophagus (when the stomach contracts, it closes off the sphincter) Indications and Pre-op Evaluation • Patients with GERD and any of the following may be considered for a fundoplication: • Erosive esophagitis, stricture and/or Barrett’s esophagus • Hiatal hernia • Dependence upon proton pump inhibitors for relief of symptoms in the absence of documented mucosal injury • Atypical or respiratory symptoms with a good response to medical treatment • Risk factors that predict a poor response to medical therapy • Nocturnal reflux on 24-hr esophageal study • Structurally deficient lower esophageal sphincter • Mixed reflux of gastric and duodenal juices Gerd Treatment Options • Lifestyle changes • Eat smaller, more frequent meals • Limit intake of acid-stimulating foods/drinks • Don’t lie down for about 2 hours after eating (or hold baby upright) • Slightly elevate head when sleeping (or bed for infants) • Maintain a reasonable weight • Don’t smoke or drink alcohol • Wear loose fitting clothing GERD Treatment Options • • • • Proton pump inhibitors H2 blockers Antacids Surgery Nissen Fundoplication • Safe and effective • 89.5% of patients are still symptom free after 10 years • Mortality rate <1% Laproscopic vs Open Surgery • 1-2 days in hospital post-op • 2-3 weeks recovery • Increased risk for difficulty swallowing • Several days in hospital post-op • 4-6 weeks recovery • Increased risk for infection and bleeding Procedure Outline 1. 2. 3. 4. 5. 6. Retract the liver Crural dissection Circumferential dissection of the esophagus Crural closure Fundic mobilization by division of short gastric vessels Creation of a short, loose fundoplication by enveloping the anterior and posterior wall of the fundus around the lower esophagus Liver Retraction • Insert liver retractor through the 10MM cannula on the patient’s right side • Position the liver retractor so that the left lobe of the liver is retracted ventrally • This exposes the anterior surface of the proximal stomach near the gastroesophageal junction Crural Dissection • Identify and preserve both vagus nerves • Open the omentum over the caudate lobe of the liver, just above the hepatit branch of the vagus nerve; this exposes the right crus of the diaphragm • Carry the incision to the patient’s left, over the anterior surface of the left crus • Dissect the right crus from its base, through the crural arch • Similarly, dissect the left crus from its base Esophageal Dissection • Gently dissect between the crura at their bases, opening the retroesophageal window • Identify and preserve vagus nerve • Pass a 1 inch Penrose drain around the distal esophagus and use it as a handle for further dissection • Dissect the distal esophagus out of the chest until at least 4 cm of distal esophagus can be pulled below the diaphragm without tension Crural Closure • Use a Maryland and a needle driver • Close the crura together using nonabsorbable sutures • Can use a bougie to measure it when completed Mobilize Gastric Fundus • Enter the lesser sac, on third of the way down the greater curve of the stomach and isolate an divide short gastric vessels, working back towards the GEJ • Divide any filmy attachments between the posterior wall of the proximal stomach and the anterior surface of the pancreas • Bring the mobilized gastric fundus through the retroesophageal window and around the distal esophagus anteriorly to ensure adequate mobilization Fundoplication • Complete the fundoplication around a 60 French esophageal dilator (inserted by anesthesiologist) • 2 or 3 non-absorbable sutures are places with bites taking full thickness gastric fundus and partial thickness anterior esophageal wall • When completed, the wrap should be no greater than 2 cm in length • Sutures from the wrap to the diaphragm are optional Operating Room Set-up: Patient • Endotracheal intubation • 30degrees reverse Trendelenburg to spontaneously lower the abdominal organs • Supine position, arms at 90degrees and legs apart • Dual lumen gastric tube to decompress the stomach; moved up to the middle third of the esophagus once the stomach has been decompressed • Surgeon stands between the legs and uses both hands Trocar Placement/Incisions • 5 total incisions • Laproscope is inserted slightly superior and lateral to the umbilicus • 4 other incisions made: 2 in upper left quadrant and 2 in upper right quadrant, bordering and inferior to the rib cage • Liver retractor goes into the incision farthest away from the surgeon on his left Instruments • • • • Liver retractor with Babcock clamp Maryland dissector Scissors Cautery or Harmonic scalpel, depending on size of patient • Needle holders Surgical Complications • Perforation of the stomach or esophagus (1% of patients) • Bleeding • Infection • About 5% of laproscopic cases result in a conversion to the open procedure Post-Operative Complications • “Gas Bloat Syndrome” – accumulation of gas in the stomach or intestine due to inability to burp (2-5% of patients) • Inability to vomit • Chest pains Post-Operative Care • • • • • • 1-3 day hospital stay Liquid diet for 1-2 weeks Rest and relax No heavy lifting No strenuous activities Expect weight loss