Esophageal Manometry
advertisement
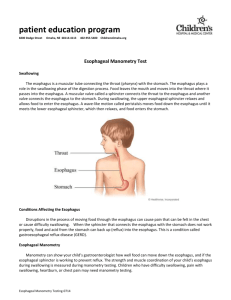
Esophageal Manometry Chhaya Hasyagar, MD Gastroenterology Kaiser, Sacramento Objectives Review esophageal anatomy Role of esophageal manometry testing Review manometry tracings Anatomy 18- to 25-cm long muscular tube cervical and thoracic parts. wall is composed of striated muscle in the upper part, smooth muscle in the lower part, and a mixture of the two in the middle. Esophageal Motility Three separate stages: – Voluntary or oral stage. – Pharyngeal stage. – Esophageal stage. Esophageal Motility Esophagus Diagnostic procedures Morphologic diagnostics – Esophageal radiography – Endoscopy – Pill cam ESO Functional diagnostics – – – – Esophageal manometry Esophageal pH monitoring Esophageal impedance Radionuclide 99 mTC scintiscanning Esophageal Manometry When does it help? – Functional disorder is suspected – Unrevealing morphological studies – Part of pre-operative evaluation Water Perfused System Water Perfused System Advantages – Cost effective – Flexibility in configuration Disadvantages – Slow response rate – Less suitable for UES and pharynx – Need for skilled personnel for use and maintenance Solid state Catheters Catheters have miniature strain gauge transducers built into the catheter to generate electrical output signals Solid State Catheters Advantages – Fast response – No water perfusion – Easy to use and calibrate Disadvantages – – – – Expensive Limited number sensors Fragile Functional lifespan Esophageal Manometry Three steps: – LES – Body – UES Esophageal Manometry ManoScan™ / HRM Overview Automatically captures all motor function from pharynx to stomach Reduces data acquisition times by more than 60% Simplifies procedures and technician training Yields portable & reproducible data sets Normal Study Using ™ ManoScan Line Trace Mode UES LES Normal study Case 1 48 year old female with long standing heartburn Symptoms well controlled on PPIs for 5 years Now with recurrence of symptoms despite high dose PPI EGD: hiatal hernia otherwise normal Esophageal manometry 24 hour pH confirmed acid reflux Proceeded with surgery for management of GERD Case 2 36 year old archeologist with gradual onset of fatigue and dysphagia. Difficulty with drinking water Returned from a trip to the Amazon basin 6 months ago EGD: Normal except for a “pop” felt while advancing scope into the stomach Next step? HREM Aperistalsis in the smooth muscle portion of the body of the esophagus. elevated resting LES pressure: >45 mmHg incomplete LES relaxation after a swallow “common channel effect” Achalasia Dilated esophagus Bird beak appearance Achalasia Idiopathic or acquired – Chagas disease Increases risk of squamous cell CA Chagas disease – parasite Trypanosoma cruzi, transmitted by “kissing bug” Achalasia - Management Endoscopic: – botulinum toxin injection of LES, pneumatic dilation of LES Surgical: – Hellers myotomy (usually with antireflux fundoplication) Case 3 50 year old female seen in the ER 4 times with sudden onset of chest pressure. Cardiac workup including stress test was negative EGD: normal Next step? Diffuse esophageal Spasm (DES) Frequent simultaneous contractions (>20-30%) with interval normal contractions. Confined distal 2/3. Multiphasic waves. Prolonged duration. Spontaneous contractions High amplitude of the contractions DES Rosary Bead or corkscrew esophagus Treatment: – – – – CCB (diltiazem) nitrates (isosorbide) Sildenafil TCA (imipramine) Nutcracker Esophagus high amplitude peristaltic contractions in the distal 10 cm of the esophagus average distal esophageal peristaltic pressures >220 mmHg Increased distal peristaltic duration (mean value >6 sec) Case 4 55 year old female with intolerance to cold, heartburn not responding to medications, with c/o dysphagia to solids for 8 months Wears gloves in summer as her fingers turn blue to purple in AC rooms Upper endoscopy: normal, no webs or rings Next step? Scleroderma Pathophysiology: – alterations of the microvasculature, the autonomic nervous system, and the immune system, leading to fibrosis – Affects lower 2/3 of esophagus Esophageal impedance Measures changes in resistance to alternating electrical current when a bolus passes through a ring Liquid containing boluses will lower the impedance to a nadir value Gas will produce a rapid rise in impedance Esophageal Impedance Esophageal motility disorders Primary disorders – Achalasia – Diffuse esophageal spasm – Nutcracker esophagus – Ineffective motility disorder Secondary disorders – Scleroderma Disclosure: none Questions