New GIT 1
Dr Basu
Part I: Oral Cavity diseases, Vocal cord, salivary
gland
Part II: Esophagus
Stomach
Dr Amitabha Basu MBBS, MD
Part I
Oral Cavity diseases, Vocal cord, salivary
gland
Oral Cavity diseases
Tumors and tumor like condition
Tumors and tumor like condition: Oral cavity
Papilloma
Leukoplakia
Epithelial tumor, Benign
lesion (a Squamous
papilloma)
Irregular white mucosal
plaque
Squamous papilloma has fibro vascular stalk
Also seen in vocal cord :
singers nodules: where
talking/ singing is a
profession !
Leukoplakia
Description → Leathery, white, discrete areas
of mucosal thickening.
Microscopy→ Hyperkeratosis + dysplasia or
carcinoma in situ of squamous
epithelium.
Risk factors →
Chronic friction, Alcohol
abuse.
Types →
Hairy leukoplakia ,
Verrucous leukoplakia,
Erythroplasia.
Hairy leukoplakia: facts
Etiology:
Almost exclusive to HIV
infection, Often EBV infection
also
Morphology:
“Hairy” white plaques on oral
mucosa caused by epithelial
thickening
Lab: CD 4 cell count (low below
200 cells/cumm).
Carcinoma of oral cavity
Risk factors →
Leukoplakia, Alcohol abuse,
Tobacco use, HPV (types 16, 18,
and 33), Protracted irritation.
Molecular
pathology
Type of
neoplasm→
Activation of cyclin-dependent
kinase.
Squamous cell carcinoma
HPV infection: koilocytosis
Squamous cells with
white cytoplasmic
vacuole and curved
nuclei
Study other similar picture
Prognosis
• Lips and early detection
– Lower lip - commonest
• 90% survive for 5 years without
recurrence.
– Floor of mouth, Base of tongue,
pharynx : Poor prognosis
Favored site for metastasis : cervical Lymph node
Neoplasms of vocal cords
• Benign: Squamous papilloma:
– in vocal cord and larynges: singers
nodule.
– HPV infection: koilocytic change.
Singers
nodule
Malignant tumor of vocal cord:
large white necrotic mass : Squamous cell carcinoma.
Salivary gland lesions
• Sialadenitis: inflammation
• Neoplasms
Sialadenitis : Etiology
• Viral
– Mumps (esp. parotids)
– Other organ
involvement in mumps
• Acute Pancreatitis (
↑ serum amylase)
• Mumps Orchitis (
infertility)
• Bacterial: due to
– Ductal obstruction
– Dehydration
• Immunological :
Sjogren's syndrome
Sialadenitis
Acute Bacterial
infection
Neutrophils infiltrating the
parotid gland.
Chronic autoimmune
(Sjogren's / Sicca
syndrome).
Dry mouth and eye
Fibrosis, lymphoid infiltrates
& Acinar atrophy.
Type of ANA present = SS-A
and SS-B autoantibody
Tumors of salivary glands
Pleomorphic adenoma
Parotid gland, and other
glands
Papillary Cystadenoma
Lymphomatosum
Or,
Warthin tumor
MOST common
Benign.
Can recur,
Malignant transformation rare
Benign, may be bilateral
Pleomorphic adenoma
• A mixed tumor
• Gross: Capsulated
• Micro:
– Chondroid region +
myoepithelial cells in
myxoid stroma
Gross and micro
myoepithelial cells
C
myxoid stroma
WARTHINS TUMOR
SECOND MOST COMMON SALIVARY GLAND
TUMOR
Gross: capsulated
Micro:
1. Double layer epithelial (oncocyte) CELLS.
2. LYMPHATIC STROMA WITH GERMINAL
CENTERS.
2 layers of oncocyte or oxyphilic cells,
lymphoid stroma
Let us relax : Part II
Esophagus
1.
2.
3.
4.
5.
6.
Tracheoesophageal fistula
Esophageal web
Esophageal Achalasia
Mallory Weiss Syndrome
Esophageal varices
Gastroesophageal reflux
1. Esophagitis
2. BARRETT ESOPHAGUS
Esophagus
Tracheoesophageal
fistula
Associated with Artesia of
esophagus.
Complication: aspiration of
gastric content after birth
and LUNG abscess.
Esophageal web
Plummer Vinson
syndrome
Weblike protrusion of
esophageal mucosa.
Morphology: Dysphagia.
Tracheoesophageal fistula
Esophageal web
Microcytic hypo chromic anemia,
chance of Cancer.
Esophageal Achalasia
Definition: Failure of relaxation of LES
Etio-pathogenesis:
Loss of ganglion cells in myenteric plexus
(often by Trypanosoma Cruzi- south America)
Gross: proximal dilatation of esophagus.
Clinical: Progressive dysplasia and regurgitation.
X- ray and gross:
rat tail (bird beak) appearance of lower esopgahous
Study other similar picture
MALLORY WEISS
SYNDROME
• Def: Longitudinal Tears of the
mucosa of esophagus at GE
Junction
• Occur after violent retching or
vomiting.
• Cause:
– Retching IN ALCOHOLIC stupor
– Also in non alcoholic without
Study other similar picture
any history [Hiatal hernia].
Clinical:
• Sudden Hematemesis: fresh blood ( usually not
profuse )
• Blood mixed with gastric contents or mucus
• Light-headedness, dizziness, or syncope
• Complication: Boerhaave syndrome (is rupture
of the esophagus- massive hematemesis may
occur )
?
Esophageal varices
• Def: Dilated submucosal esophageal veins
in lower third of esopgahous .
• Cause: Portal hypertension following
alcoholic cirrhosis.
• Effect: Result in massive upper GI
hemorrhage when ruptured.
Gross and micro
Dilated and
thrombosed vessels on
the sub mucosa
Gastroesophageal reflux disease
• Etiology: Sliding Hiatal hernia and
incompetent lower esophageal sphinter,
alcohol, Scleroderma.
• Complications: Reflux Esophagitis, Barrett
esophagus
• Clinical: heart burn , relieved by antacids.
BARRETT ESOPHAGUS
• Morphology: columnar epithelial
metaplasia of esophageal
squamous epithelium.
• Complications: esophageal
adenocarcinoma (lower 1/3rd of
esophagus).
Columnar epithelial metaplasia with goblet cells
or, Intestinal metaplasia → adenocarcinoma
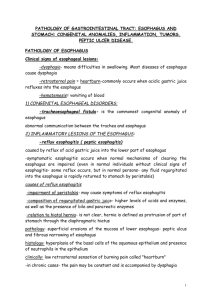
Esophageal Squamous cell Carcinoma
Etiopathogenesis
Type of tumor
Morphology
Clinical
Alcohol, tobacco, HPV ( High
risk groups), smoking.
Squamous cell carcinoma
Upper 2/3rd of esophagus.
Gross: tumor with central
necrosis and microscopy of
SCCA
Progressive weight loss,
dysphagia.
Study other similar picture
central necrosis
End of esopgahous
Disease of Stomach
Stomach
•
•
•
•
•
Pyloric stenosis
Menetrier disease
Gastritis
Peptic ulcer
Malignant tumors
Pyloric stenosis
•
•
•
•
Congenital.
More in male
Cause: hypertrophy of the circular muscle
Clinical:
– Outlet obstruction, Projectile vomiting.
– First 2 weeks of life.
– Oval mass upper abdomen.
– Association with Turner syndrome (45, X0)
/ Edward syndrome (Trisomy 18).
Multifactorial inheritance
• If present in female – more chance (than
male) that she will pass this disease to her
offspring.
• So, If a child with PS is female:
– the likelihood of having a future son with PS is
one in five.
– the likelihood of having a future daughter with
PS is one in 14.
Gastritis
• Acute hemorrhagic gastritis
• Chronic gastritis
Acute hemorrhagic gastritis
Def: acute inflammation, erosion and
hemorrhage in present in gastric
mucosa.
Cause : aspirin, NSAIDs, smoking, burns,
brain injury, stress, uremia, post surgery.
Gastric erosion: acute gastritis
Time for chronic gastritis
Chronic inflammation → atrophy of
gastric mucosa = atrophic gastritis
Autoimmune gastritis
Pernicious anemia:
site: fundus
Reduced acid secretion
• Auto-antibodies to parietal
cell or intrinsic factors are
present in the serum.
• Megaloblastic amenia.
•Peripheral (nerve) myelin
loss.
Helicobacter pylori
associated gastritis
Site: antrum
Curved, gram
negative and silver
stain (GMS) positive
rod
In duodenum
Autoimmune gastritis
• Atrophic gastric mucosa + intestinal metaplasia
(goblet cells) + few lymphocytes
Increased chance of gastric carcinoma
Helicobacter pylori associated gastritis
• Mucosa shows acute and chronic inflammatory
cells+ atrophy + silver stain positive curved
organism
↑ chance
of. both gastric carcinoma / lymphoma
Peptic ulcer
•
•
•
•
•
Location
Etiology
Pathogenesis
Morphology
Complication
Peptic ulcer
Peptic ulcer of the duodenum
• Location:
1. Duodenum : first portion [
common]
2. Stomach, usually antrum
3. In Zollinger-Ellison syndrome
[multiple non healing ulcers]
4. Meckel diverticulum that
contains ectopic gastric
mucosa.
Etiology and pathogenesis
1.
Etiology:
1. H. pylori ( more with duodenal ulcer than gastric
ulcer), chronic use of NSAIDs, Aspirin, Cigarette
smoking, Corticosteroids.
2.
Pathogenesis:
• Increased secretion of hydrochloric acid and pepsin
and reduced mucosal defence.
Duodenal peptic ulcer- DU
• More common than gastric
• Etiology :
– H.pylori (100%), Blood group O
– Zollinger-Ellison syndrome ( gastrinoma):
multiple non healing ulcer.
– Increased gastric emptying
• Location: Anterior wall: first portion of duodenum
• C/F: Pain which is relieved by food.
Gastric ulcer
Benign or
Malignant?
Small, oval ( 1-3 cm), single
Punched out margins
Clean ulcer base
C/F: Pain aggravated by food.
Benign vs malignant gastric ulcer
Small, oval ( 1-3 cm),
single
Punched out margins
Clean ulcer base
Large
Rolled up ( heaved up)
margins
Necrotic base
Complications: Peptic ulcer
• Bleeding: more with DU
• Perforation: more with DU
• Obstruction : due to edema and scarring:
more with DU
• Cancer: more with gastric ulcer.
Time for gastric tumors
Menetrier disease
Adenocarcinoma
Menetrier disease
• Enlarged gastric rugal foldlike brain.
• Massive foveolar
hyperplasia
• Reduced gastric acid
• Reduced serum protein (
protein loosing
enteropathy- edema, low
plasma protein).
Gastric tumors: facts
• Age: >50 years
• Sex: Men, Blood Group A: frequent
• Geographic Location: More in Japan,
Finland, Iceland, less in USA.
• Anatomical location: The lesser curvature of
the antropyloric region.
Etiology: Gastric CA
1. H.Pylori (Chronic atrophic gastritis)
2. Nitrosamine: smokes fish and vegetable,
pickle ( preservative > Japan).
3. Increased salt and low fresh food intake.
Morphology
Adenocarcinoma ( always)
• Early
– Early gastric carcinoma-is defined as a
lesion confined to the mucosa and
submucosa.
• Advanced
– neoplasm that has extended below the
submucosa into the muscular wall.
Morphology of advanced Gastric carcinoma
• Gross
Micro
Etiology
Exophytic
( polypoid)
Intestinal type of
malignant glands
Associated with
Infiltrating or
diffuse
Signet ring cells in
all layers of
stomach
Not associated
with H.Pylori
H.Pylori
Intestinal type of malignant glands
Infiltrating or diffuse
• Also known as: linitis plastica
• Diffuse infiltration of malignant cells in the
stomach.
• Produce ‘leather bottle’ stomach: small
shrunken stomach.
linitis plastica
Diffuse type: signet ring cells
(contain mucin in the cytoplasm): poorly differentiated
Other facts
• Metastasis
– To the left supraclavicular sentinel
(Virchow) node: hypothetical first lymph
node.
• Metastasize to both ovaries : Krukenburg
tumor.
• Prognosis: poor
• Hematemesis and melena- black stool +.
Prognosis depends on Grading
• Well differentiated tumor : well formed glands, small
in size, less mitosis : good prognosis.
• Moderate differentiated (more irregular glands but
still identifiable) : intermediate prognosis.
• Poorly differentiated (predominant unrecognizable
glands and cells): bad prognosis
• Undifferentiated : barely recognizable primary
tissue: very bad prognosis
• Anaplastic: bizarre and large cells, more mitosis:
worse prognosis
Thank you