coronary_circulation..
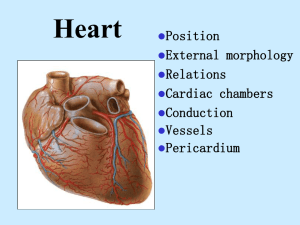
advertisement

1650= Vieussens described first. 1799=Edward Jenner established the relationship between the coronary artery and angina pectoris. 1809=Allan Burns described the same. 1958=Maron Sones performed the first selective coronary arteriography. 1968=Rene Favalan and Dudley Johnson introduced the coronary artery bypass surgery. Coronary vascular endothelial maturation-closely parallels the development of embryonic epicardium. Heart begins to pump blood before perfusion of the coronary vasculature occurs-early trabecular myocardium is metabolically supplied by local diffusion of nutrients.This fact-made use of in endocardial laser revascularisation procedures for angiographically proved extensive disease of the coronary arteries, where CABG is not feasible. Neural crest ablation-marked abnormality of coronary vessel development. Coronary arteries-2 in no. arise from evaginations,coronary sinuses at the root of aorta. Left-from left coronary sinus & Right-from right coronary sinus.The third evagination-non-coronary sinus. Two major and two minor loops. Major loops-situated along the interventricular and AV grooves. Minor loops-around the right ventricular conus and the sinoatrial region. Architectural pattern 1. 2. 3. Epicardial or conductance vessels. Intramyocardial or resistance vessels. Subendocardial plexus of vessels. Left coronary-coronary sinus-LAD & circumflex arteries. LAD= in the interventricular groove till the apex-supplies about 50% of the LV mass and a small strip of the adjoining right ventricle. Branches: a) Septal perforators- supply inter-ventricular septum. b) Diagonals-supply the remaining LV mass. Circumflex= travels in the left AV groove,finally reaches the crux on the posterior aspect of the heart. Branches: a) obtuse marginals=1-4 in no. and supply the lateral wall of the left ventricle. Left main=sometimes trifurcates. Intermediate artery-supply similar to 1st diagonal. RCA= rt.coronary sinus-right atrioventricular sulcus.-crux-meets terminal portion of circumflex. Right dominant= posterior descending artery from RCA, travels in the posterior interventricular groove. Left dominant=PDA from the circumflex. Branches of RCA: a) conus a.-meets a branch from LAD around the conus of the right ventricle-one minor loop of the coronary circulation. b) sinus node a.->50%=from RCA-opposite direction of conus a.encircles the SVC-rt. Atrial junction-second minor loop. c) acute marginal branch=travels along the lower border of rt. atrium. d) posterior descending artery=terminal portion communicates with the terminal portion of the LAD artery around the apex.Where there is a major blockade of the LAD, a patent right dominant system can supply the LAD region in a retrograde way. LV= 50% from the LAD. 25% from the left circumflex, 25%posterior descending a.(from rt. Coronary or the left circumflex). . The anterolateral papillary muscle-blood supply from the diagonal branches of LAD. The posterior papillary muscle-dual blood flow from circumflex and terminal branches of RCA. Sinus node-In majority by RCA, in a small proportion by the circumflex. AV node-The first posterior perforator of the PDA. Bundle of His-dual blood supply from both the PDA and LAD, more resistant to ischemia than the AV node. Rt. Bundle-LAD and RCA. Left bundle-mainly from the diagonals. RV=Anterior portion adjacent to the interventricular septum-branches of LAD.Rest-RCA. In left dominant-posterior portion -circumflex. RA-RCA. LA-Left circumflex. An extensive intercommunicating network by a. the coronary sinus b. the anterior right ventricular veins. c. the thebesian veins. Coronary sinus= in the left posterior AV groove-drains predominantly the left ventricle and the left atrium. Tributaries:a)The anterior inter-ventricular vein-ends as great cardiac v b) The middle cardiac vein-from the posterior interventricular region. c) the oblique vein of Marshell-from the posterior aspect of left atrium. - opens into the rt.atrium between the orifice of IVC and septal tricuspid leaflet. The anterior cardiac v.-2-4 in no. They drain the anterior right ventricular wall and end at the base of the right atrium. The small cardiac v.-receives from rt.atrium and opens into RA. The thebesian veins-tiny venous outlets draining the myocardium directly into the cardiac chambers(rt. Atrium and rt.ventricle). INNERVATION Sympathetic: from superior,middle and inferior cervical ganglia+upper 5 ganglia of the symp.chain. Para-symathetic: nodose ganglion. At the heart, both mingle to form cardiac plexus-superficial and deep portion. Compared to the symathetic, the parasympathetic innervation is sparse. 5% of the blood flow of the total cardiac output(250-275ml/min). AV oxygen content difference=10 ml/100 ml(5 ml/100 ml in other vascular beds). During exercise, the values are the same. Oxygen consumption-25 ml/min.(beating heart at rest). -6 ml/min(non-beating heart). -0.12 ml/min(for electrical activation)] Anatomical factor: arranged as a) epicardial conductance vessels (constrict to alpha stimulation and dilate to NTG.) b) intramyocardial resistance vessels(at right angles to the above). c)subendocardial plexus of vesselsdense capillary network of about 4000 capillaries/sq.mm, not uniformly patent-pre-capillary sphincters serve a regulatory roleopens out when myocardial demand increases. Perfusion pressure: LV perfusion pressure= aortic diastolic pressure- LV end-diastolic pressure. All organs are perfused during systole except the LV(since the resistance vessels are compressed during systole). RV-thinner ventricle. Receives its major blood flow during systole. Under basal conditions, blood flow to the subendocardium/subepicardial layer=125:1 (maximal preferential dilatation of the subendocardial plexus of vessels. Significance: In the presence of a significant coronary artery obstruction, subendocardial vessels can’t dilate further and suffer the most by way of ischemia. Collaterals: Anastomotic connections between portions of the same coronary artery and between different coronary arteries-diameter-40200 µ. Open out only with repeated brief periods of ischemia.With sustained partial occlusion-collateral blood flow commences in 5-10 min. and progressively increases for 24 hrs.In 6-12 months time , they acquire an organised smooth muscle coat.They are influenced by external influences. Significance: No anginal pain even with 80-90% obstruction of a major vessel but when demand is increased, collateral circulation may be inadequate. Local metabolism: primary controller. Local arterial vasodilatation in response to muscle need for nutrition. Chemical agents resposible are: a) adenosine b) potassium ions c) hydrogen ions d) bradykinin e) prostaglandins.PGI2 and PGE2. Oxygen lack: opening of ATP dependent K+ channels-hyperpolarization- Ca2+ channel opening prevented-vasodilatation. Auto-regulation:At perfusion pressures from 60-130 mm of Hg, CBF is the same(myogenic, metabolic factor and release of endothelial vaso-active factors are implicated). Neural factor: α-vaso-constriction ß-vaso-dilatation. Para sympdilates Endothelial control: EDRF(released by several stimuli), prostacyclin, endothelin. Reactive hyperemia Coronary flow reserve Coronary steal Myocardial stunning Myocardial hybernation Deteminants of Myocardial oxygen demand & supply Supply ↓: a) Coronary stenosis Demand ↑: a)Heart rate b) Coronary perfusion pressure↓ b)contractility c) ↓coronary perfusion time c)ventricular d)↓Hb wall tension e)↓PaO2. d)ventricular cavity radius