Coronary Disease Overview
advertisement

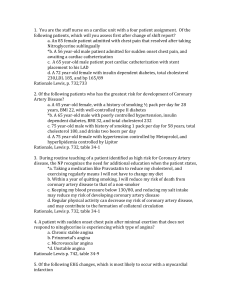
CORONARY ARTERY DISEASE OVERVIEW Pathogenesis, Clinical Features, Diagnostic Testing and Therapy Hank George, FALU, CLU, FLMI “Myocardial infarction, sudden death and unstable angina have in common a genesis of coronary thrombosis, which develops as a result of a ruptured vulnerable or an eroded atherosclerotic plaque. As long as atherosclerotic lesions do not rupture and eroded plaques do not induce thrombosis, coronary disease may be a clinically silent disease associated with low mortality. Whenever plaques start to rupture and thrombogenic material is coming into contact with circulating blood, a situation is created which may lead to acute coronary syndrome associated with high mortality” Johannes A. Schaar Erasmus Medical College, Amsterdam Circulation 108(2003):2636 What do we know about atherosclerosis? • It is a diffuse, systemic disease of the arterial tree • It may be present and even severe despite the absence of recognized clinical symptoms • It may produce no extra mortality or morbidity…until it destabilizes resulting in VULNERABLE PLAQUE What characterizes a VULNERABLE PLAQUE? Typically, a non-obstructive atheroma having a central lipid core, a thin fibrous cap and a yellowish appearance. What can trigger an acute coronary event by inducing destabilization of a vulnerable lesion? • • • • • • • • • • Temperature change Smoking a cigarette Sexual activity Vigorous exercise in a deconditioned person Acute mental stress Pollution Infection Excess hydration Day-to-day dietary changes Severe periodontal disease What is the “endothelium?” The lining covering the internal surface of blood vessels, heart valves and bodily cavities What is the role of the endothelium? It protects the artery from injury by maintaining an antithrombotic surface, mediating vasodilation and inhibiting inflammation What is endothelial DYSFUNCTION? Disruption of normal function, leading to vasoconstriction, endothelial inflammation and thrombus formation What induces DYSFUNCTION? Inflammation, excess oxidized LDL-cholesterol and many other complex biological factors How do we know that inflammation occurring outside the coronary arteries is associated with acute coronary syndromes? Because patients with systemic inflammatory diseases such as rheumatoid arthritis and SLE develop endothelial dysfunction and have excess CAD Coronary Artery Disease Four Main Presentations SILENT ISCHEMIA CHRONIC STABLE ANGINA PECTORIS ACUTE CORONARY SYNDROMES UNSTABLE ANGINA PECTORIS MYOCARDIAL INFARCTION SILENT ISCHEMIA • Ischemic changes on ECGs in the absence of clinically-recognized symptoms • Most common in diabetics due to neuropathy • As significant as chronic stable angina in terms of the subsequent risk of ACS events, as well as mortality and morbidity. CHRONIC STABLE ANGINA • Episodes of chest pain and other symptoms (dyspnea, fatigue) induced by increased oxygen demand and relieved with cessation of inciting activity or Rx • Patients often have 2-3 times more silent episodes than symptomatic episodes • BEST CASES have minimal excess mortality when compared to the general population How does chronic stable angina differ from unstable angina? STABLE • Presents with typical chest pain, induced by typical symptoms • May be presumptively diagnosed by symptoms only • Due to fixed obstructive disease • Managed as outpatient • Treated medically or surgically – often by patient choice UNSTABLE • Presents like MI with prolonged chest pains, etc. • Diagnosed by ECG and cardiac markers • Due to intraluminal thrombus formation in vulnerable disease • Managed in hospital • Treated by percutaneous coronary intervention (PCI) CHEST PAIN EPISODE Underwriting Triage • Age, gender • CV profile • Where did patient present? ER? GP office? • Were Sx typical or atypical • What brought it on? • What brought relief? • Referral to non-cardiologist? • Management TROPONIN • Myocardial proteins cTnT + cTnI • Essential component of MI diagnosis • Elevate from heart muscle damage; more sensitive and specific than CK-MB • Degree of elevation during/after MI key to long term prognosis • Elevates in other scenarios, including after noncardiac surgeries • These elevations are adverse mortality predictors even in absence of structural/functional heart damage NT-proBNP Finest CV Marker EVER • Elevations due to myocardial stretch • Elevates in all forms of cardiac disease • Predictive of future mortality in subjects free of known CV disease • Independent of usual CV risk factors • Inexpensive • Recent report says protective value payoff from this test is FANTASTIC • Will replace subjective (treadmill, ECG) CV screening in underwriting Other candidates for CV screening • HbA1-c • Cystatin C • Apolipoprotein B:A1 ratio Diagnostic Testing in CAD • Resting ECG • Treadmill stress ECG • Stress echocardiogram – exercise vs. dobutamine (why can’t he exercise?) • Myocardial scintigraphy (thallium, etc.) • Noninvasive CT angiography • Invasive angiography (presurgical?) Disease Assessment Parameters • • • • Exercise ischemia Treadmill performance Reversible vs. irreversible lesions Left ventricular ejection fraction (LVEF) • Wall motion: hypokinesis, dyskinesis, akinesis • Degree of fixed obstructive disease CAC Coronary Artery Calcium • Scanned for with helical and electron beam computed tomography • Extent of calcium quantified • Range 0-400 • Very low risk with scores 0-10; just the opposite with 101-400 • Readily available to consumers for $200 = antiselection potential! MEDICAL MANAGEMENT • Antianginals: nitroglycerin, isosorbide dinitrate, mononitrates • Beta-blockers or calcium channel blockers as alternative antianginals • Clopidogrel, aspirin as antithrombotic prophylaxis • Statin prophylaxis • Lifestyle modification SURGICAL MANAGEMENT • Percutaneous coronary intervention, with or without stenting (PCI) • Coronary artery bypass grafting (CABG) • CABG has less long-term cardiac morbidity in terms of symptom recurrence • No difference in 10 year prospective mortality Bravata. Annals of Internal Medicine. 147(2007):703 Does surgical management lead to lower subsequent mortality than medical management? It depends on which study you believe! Overall, this does not matter nearly as much as (1) the extent of heart damage and (2) how the patient responds to the diagnosis in terms of compliance and lifestyle choices What factors should be considered in potentiallyinsurable CAD cases? • Extent of myocardial damage • Current myocardial function, based on interim testing • Nature and extent of treatment • Compliance with Rx • Risk factor improvement (BP, lipids) • Health habit changes (quit smoking, exercise)…and …one more: whether or not the individual is depressed, based on symptoms, need for treatment, etc. Many recent studies have shown that depressed CAD patients have significantly greater intermediate and longer-term morbidity and mortality CHEST PAIN with normal coronary anatomy • • • • Mostly women Chest pain has features of angina Often positive stress test Further evaluation shows no evidence of significant obstructive coronary disease • Microvascular disease often present • No significant extra mortality • Substantial excess morbidity STRESS CARDIOMYOPATHY • Takotsubo cardiomyopathy, apical ballooning syndrome • 82% postmenopausal females • Induced by severe stress, also acute medical illness and after surgery • Presents like ACS • No obstructive lesions • Normalization of left ventricular function in 1-3 months in most cases • Supportive care only • Recurrence rate 2-10% What is the long-term mortality risk?