Pathophysiology of Coronary Artery Disease
advertisement

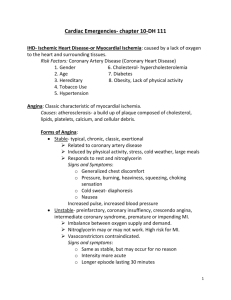
Pathophysiology of Coronary Artery Disease Blood supply to the heart Coronary Blood Flow: Constant Demand Arteries & veins are located on the surface of the heart, lying within groves called sulci Blood flows through coronaries during the RELAXATION phase (diastole) Why? Primary Superficial Arteries Right Coronary Right Marginal Branch Left Coronary Left Anterior Descending Left Circumflex Areas of Coronary Artery Perfusion: LAD: Majority of the left ventricle: Anterior/Inferior Circumflex (Cx): Inferior and Posterior LV RCA: RV, Posterior and Septal Circumflex LCA LAD Right Marginal Branch RCA Rt. Marginal Pathogenesis of Atherosclerosis Step 1: Endothelial Injury Location? coronaries, carotids, renal arteries, lower extremities Tunica Intima damaged (How?) LDL Oxidation: Initiates Inflammatory Process: Monocytes: Attracted and “glued” to endothelium by “ELAMS” (endothelial-leukocyte adhesion molecules) STEP 2: Inflammation gone Haywire Monocytes/Leukocytes enter the Sub-endothelial space Initiate Smooth Muscle Cell proliferation Attract more LDL to create a “fatty streak” Ouch! Blood Clot Normal Narrowed Occluded LDL’s and Atherosclerosis Oxidized LDLs act as a “free radical”, which induces endothelial injury inflammation begins Some LDLs are removed by macrophages, but high LDLs will cause much injury LDLs = accelerated atherosclerosis Vessel Lumen Smooth Muscle Myocardial Oxygen Supply Cardiac cells extract most of the oxygen delivered (high A-vO2 diff) Thus additional oxygen can only be met by delivering more blood by the coronary arteries A reduction in coronary artery lumen size attenuates blood flow Degree of Occlusion & Blood Flow Blood Flow 25 50 75 100% Blood Flow Big reduction beyond 75% occlusion Severity of disease depends on # of occluded arteries Also location of occlusion (left coronary vs apical) Myocardial O2 demand (MVO2) depends on.. Myocardial tension (pressure x volume) Inotropic State (Measure?) Chronotropic state (Measure?) Myocardial mass Indirect measure of MVO2 Rate pressure product (a.k.a. double product, tension-time index) Considers 2 of the MVO2 indices: HR X SBP Good estimate of oxygen use by the heart. Used to determine angina threshold End Results of Atherosclerosis Unstable Angina Stable Angina Acute Myocardial Infarction Sudden Cardiac Death Stable Angina Angina occurs at a consistent and predictable level of MVO2 Reduced Coronary Blood Flow Always exercise at an intensity below the angina threshold How would you identify the angina threshold? Anginal Symptoms Varied: Chest pressure/heaviness Back, neck, shoulder ache Diaphoresis Pallor Dyspnea Does it occur upon exertion? Unstable Angina Due in part to intra-coronary spasm This reduces lumen diameter May occur ANY time (unpredictable) and at any work intensity Termed “Vasospastic” or “Prinzmetal’s Angina” Acute Myocardial Infarction Intra-lumenal thrombus formation Thrombus lodges in coronary artery, stops blood flow Cells downstream are starved of O2 Leads to tissue necrosis LAD: Thrombosis Area of Infarct Sudden Death May be due to the death of heart tissue from large vessel occlusion or.. emboli (ischemia) induce ventricular arrhythmias that will kill (i.e. ventricular fibrillation) Infarction symptoms Similar to angina: diaphoretic, pallor complexion, pain Vomiting, dyspnea Symptoms are often ignored or denied by the patient Odds of survival are greatest if they get help within 1 hour Complications of MI Cardiac Tamponade: Fluid between pericardium/myocardium Pericarditis: Inflammation of the pericardium Emboli: From either MI thrombus or atrial clots formed with atrial pooling Most Common Complications: Congestive Heart Failure: 75% of MI’s experience overt CHF Fluid backs up… 25% of MI’s experience “compensated” CHF reduced perfusion to “vital organs”? Dysrhythmias: The importance of ECG monitoring post-MI Assignment: Read: “Cardiovascular disease and the endothelium” Answer: How does understanding the mechanism of the disease (pathophysiology) improve prevention, detection and intervention strategies?