Staged PCI in a patient with multivessel coronary disease
advertisement

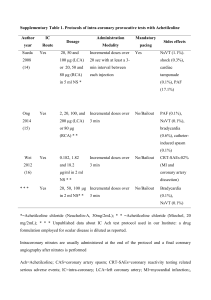
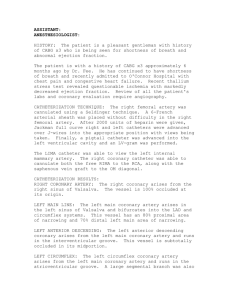
Call for CASES Staged PCI in a patient with multivessel coronary disease disqualified from CABG. Pawel Buszman, MD, FESC, FSCAI Marcin Debinski, MD Krzysztof Milewski American Heart of Poland, Ustron, Poland & CCU, Upper-Silesian Heart Center Silesian Medical School Katowice, Poland Introduction • PCI and CABG offer similar long term results (in respect to MI and death) in patients with moderately advanced coronary artery disease (CAD). • There are very few information on effectiveness of PCI in patients with diffuse CAD and high risk of surgical intervention. • Technological progress in interventional cardiology together with advances in pharmacology should result in better outcome in patients with end stage coronary artery disease. Description of the problem • Male, 76 years old • Unstable Angina, class CCS IV • Medical history: 2xMI (1994-nonQ anterior, 2003-inferior wall) • CAD Risk factors: HA, family history, former smoker • LVEF 40% • EUROSCORE 13 points: – age 4 pt – unstable angina after AMI 2 pt – peripherial atherosclerosis – paroxysmal FA – chronic obstructive pulmonary disease – respiratory insufficiency 2 pt 3 pt 1 pt. 1 pt. Description of the problem Coronary arteriography: RCA: 60% stenosis in prox. RCA, 99% narrowing in med segment LCA: LM-diam. ca 3.5-4 mm, length 15mm, LAD-30% prox.lesion; critical, long, calcified, tortous lesions in med and distal LAD, Cx-90% type A lesion in prox, 99% type B2 lesion in distal segment. RCA LAO60 LCA: RAO 30 LCA: LAO60/cran25 Intended strategy • Multiple, stage PCI with continous control of previously dilated vessels/segments. • Use of bare metal stents to minimize costs of procedures. • Carefull evaluation of contrast volume used for each procedure and renal function before/after eache stage. • Concomitant pharmacological treatment: ASA 150mg o.d., clopidogrel 75mg o.d., ACEI, selective beta-blocker, statins, First stage Aug’2003: Predilatation of critical lesion in med RCA (balloon 3.0x20mm) and stenting of prox/med. segment (stent Chopin, Balton, 3.5x34mm, 18 atm). No complications. Hospitalization 6 days. Right coronary artery (RCA) in LAO 60, before and after PTCA. Second Stage Sept’2003: RCA: non-significant narrowings in med segments. PCI to Cx: POBA of distal lesion and predilatation and stenting of prox lesion (Chopin 3.0x8mm, 18 atm.) No complications. Hospitalization 3 days. Fig 1. Left coronary artery (LCA) in LAO 60, before and after PCI to Cx. Third Stage Dec’2003: RCA: patent and large vessel, non-significant narrowing in med segments. Cx: restenosis in distal segment (75%). PCI to LAD: predilatation (balloon 1.5x20 & 2.0x20mm) and stenting of med/distal LAD (Multilink Zeta, 18 atm.). VF during stent implantation, successfully defibrillated within 15 s (1x300W). No further resuscitation or intubation required. PCI to Cx: POBA of distal restenotic lesion (balloon 2.5x20mm), residual stenosis<30%. Lab tests: Troponin I 1.04ng/ml; CK 337 U/l, CKMB 31 U/L. Hospitalization: 4 days. Third Stage Fig 1. Left coronary artery (LCA) in LAO 60, before and after PCI. Fourth Stage March’2004: A control angio revealed patent coronary arteries without significant stenosis. RCA: LAO 60 LCA: RAO 30 LCA: LAO20/cran25 Follow-up 9 • • • • • months after the first stage we noticed: No significant stenosis in coronary arteries LVEF improvement (55%) Decrease of angina symptoms (CCS I) Improvement in quality of live, NYHA class II No further intervention requiered. Further intensive pharmacological treatement: statins beta-blocker ACEI ASA Conclusions • Stage PCI is a rational alternative to CABG in patients with advanced coronary artery disease and high risk of perioperative complications. • In patients undergoing POBA or bare metal stent implantation a routine follow-up angio should be considered. • Stage PCI offers opportunity to review previously dilated/stented coronary segments. It may limit obligatory use of DES.