Acute Abdominal Pain In Children
advertisement
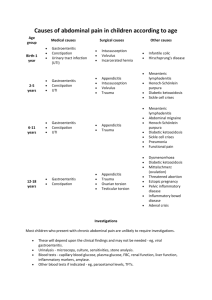
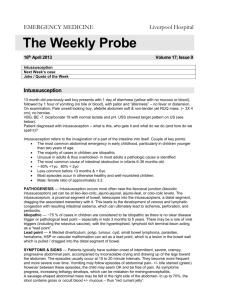
Acute Abdominal Pain In Children Hai Ho, M.D. Department of Family Practice Pathophysiology of pain • Visceral pain – Mechanical – stretching – Chemical – mucosa – Aching and dull, poorly localized • Parietal pain – Sharp, well-localized Pathophysiology of pain • Referred pain – Somatic and visceral afferent fibers enter the spinal close to each other • Localization of pain – Bilateral – most GI tract, midline pain – Unilateral – kidney, ureter, ovary, somatic History • Usual: quality, location, severity, associated symptoms, aggravating/alleviating factors • Kids cannot give a history • Dangerous signs given by parents My history: the red flags • Duration – acute vs. chronic • Fever – inflammation, infection • Vomiting – stasis, obstruction, dehydration • Urine output – volume depletion • Diarrhea - bloody Examination • Usual: inspection, auscultation, percussion, palpitation • Rectal – rectocecal appendicitis, occult blood • Pelvic – PID • Scrotal - torsion Tests? • Chemistry – electrolyte abnormality, BUN/creatinine, liver function test • CBC – infection, bleeding • Plain abdominal x-ray – free air, obstruction • Urinalysis – pyuria, hematuria • Pregnancy test Pyloric stenosis What is pyloric stenosis? Hypertrophy of pylorus – thickening & elongation Cause of pyloric stenosis? • Unknown • Associations – Abnormal muscle innervations – Erythromycin in neonates for pertussis postexposure prophylaxis – Infant hypergastrinemia Epidemiology • Prevelance – 3/1000 • More common in white northern European descents • Male:female = 4:1 to 6:1 • Age – 1 week – 5 months but usually 3 to 6 weeks Clinical presentation? • Abdominal pain • Nonbilious vomiting after feeding and with 91% having projectile emesis Distinguish pyloric stenosis from GER? Clinical presentation? • Abdominal pain • Nonbilious vomiting after feeding and with 91% having projectile emesis – Hungry after feeding – Weight loss – Progressive symptoms Clinical presentations • Jaundice – 5% of affected patients – Indirect hyperbilirubinemia due to decreased level of glucuronyl transferase Examination? • Abdominal distension • Olive mass – RUQ, after feeding Examination • Gastric peristaltic wave from left to right after feeding Tests? • • • • Chemistry Plain abdominal x-ray Ultrasound UGI Chemistry? • Decreased chloride • Elevated bicarbonate – metabolic alkalosis • ± Hypokalemia • Elevated BUN and creatinine • ±Elevated indirect bilirubin Abdominal x-ray Increased gastric air or fluid suggestive gastric outlet obstruction Ultrasound • Pyloric length > 1519 mm • Wall thickness > 34 mm • Pyloric diameter >10-14 mm Ultrasound Shoulder sign indentation of pylorus into the stomach UGI • String sign • Pyloric spasm may mimic the string sign Treatment? • Medical resuscitation first – IVF hydration with potassium – Correction of alkalosis because of postoperative apnea associated with general anesthesia • Pyloromyotomy • Endoscopically-guided balloon dilation – surgery is contraindicated or incomplete pyloromyotomy Pyloromyotomy Pyloromyotomy Pyloromyotomy: laparoscopy Postoperative management • May be fed within 12-24 hours, early as 4 hours post-op in one study • Vomiting – Not a reason to delay feeding – GER – up to 80% post-op – Consider UGI if vomiting persists > 5 days Intussusception What is intussusception? Invagination of intestine into itself Pathophysiology • Proximal bowel telescopes into distal segment, dragging along mesentery • Compression of mesenteric vessels & lymphatics leads to edema, ischemia, mucosal bleeding, perforation, and peritonitis Ileocolic intussusception Causes of intussusception? • Idiopathic – – 75% of ileocolic intussusception – More likely in children < 5 Causes of intussusception • Leading point – Hyperplasia of Peyer patches in terminal ileum – Structural: small bowel lymphoma, Meckel diverticulum – Systemic: cystic fibrosis, HenochSchönlein, Crohn disease Epidemiology • Male:female – 3:2 • Age – – 3 months to 6 years with 80% < age 2 – Peak at 6-12 months • Most common - ileocolic Clinical manifestations? • Intermittent, severe, crampy abdominal pain with loud cry and in curled up position • Vomiting • Appear normal between attack • Currant-jelly stool Currant-jelly stool Mixture of blood and mucus Foul smelling Tests? • Chemistry – dehydration, electrolyte imbalance • CBC – infection • X-ray: plain film & contrast or air enema • Ultrasound • CT scan – only if other tests are negative X-ray : plain film X-ray • Contrast material between the intussusceptum and the intussuscipiens is responsible for the coil-spring appearance • Use water-soluble agent prior to barium if high risk of perforation suspected Ultrasound Could detect ileoileal intussusception Treatment? • Air or contrast reduction – Air is better than barium reduction – less perforation <1% – Not very successful if symptoms > 24 – 48 hours or with bowel obstruction – Successful rate – 75-90% with ileocolic intussusception • Surgery Reduction Surgery • Manual reduction and end-to-end anastomosis • Indications – Persistent filling defects – Failed nonoperative reduction – Prolonged intussusception Recurrence • 10% • Not necessary an indication for surgery Malrotation & Volvulus Normal development Midgut volvulus Volvulus Cecal volvulus Sigmoid volvulus Clinical presentation? • Bilious emesis • Abdominal distension Tests? • UGI- duodenum not crossing the midline • Barium enema – malposition of cecum Abdominal series Gastric and duodenal bulb distention Little air in intestine UGI with SBFT Cork-screw pattern – barium flowing through restricted bowel lumen Treatment: surgery