Advanced Practice of Pharmacy Experience: Journal Club Mai Nguyen

Title
Clinical
Trial
Rivaroxaban Versus Warfarin in Nonvalvular
Atrial Fibrillation
Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition
Compared with Vitamin K Antagonist for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF)
Authors Patel MR, Mahaffey KW, et al.
Citation
Funding
Patel MR, Mahaffey KW, et al. Rivaroxaban versus Warfarin in
Nonvalvular Atrial Fibrillation. New England Journal of
Medicine. 2011;365:883-891.
Johnson & Johnson Pharmaceutical Research and
Development
Bayer Healthcare
Atrial fibrillation is associated with an increase in the risk of ischemic stroke by a factor of 4 to 5 and accounts for up to 15% of strokes in persons of all ages and 30% in persons over the age of 80.
1
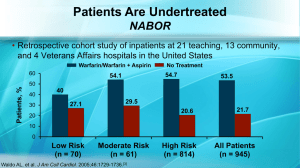
Current guidelines for preventing stroke in patients with atrial fibrillation recommend using warfarin, a vitamin K antagonist, with a target INR of 2-3, as the standard care of therapy.
However, warfarin has many food and drug interactions, and requires frequent monitoring and dose adjustments.
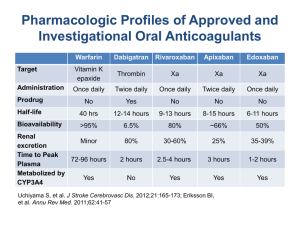
Rivaroxaban (Xarelto®):
3
First oral, selective inhibitor of Factor Xa approved by the FDA on July 1, 2011.
FDA indicated for prophylaxis of deep vein thrombosis (DVT) which may lead to pulmonary embolism (PE) in patients undergoing knee or hip replacement surgery.
Convenient once daily, oral dosing
No need for routine monitoring of INR or other coagulation parameters.
To compare once daily oral rivaroxaban with dose-adjusted warfarin for the prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation who were at moderate to high risk for stroke.
Primary hypothesis: rivaroxaban is noninferior to warfarin for the prevention of stroke or systemic embolism.
Trial Design
Prospective, multicenter, double-blind, randomized eventdriven trial
14,264 participants underwent randomization from
December 18, 2006, through June 17, 2009.
The study was terminated on May 28, 2010.
Setting
Study was conducted at 1,178 sites in 45 countries.
Inclusion Criteria:
Men or women aged ≥ 18 years with nonvalvular atrial fibrillation (ECG evidence), who were at moderate-to-high risk for stroke.
▪ Elevated risk factors: history of stroke, transient ischemic attack, or systemic embolism OR
▪ At least 2 of the following risk factors: heart failure or left ventricular ejection fraction of ≤ 35%, hypertension, age ≥ 75 years, or DM
Female subjects must be postmenopausal, surgically sterile, or abstinent.
▪ If sexually active, must use effective method of birth control before entry and throughout the study.
▪ Must have a negative pregnancy test at screening.
Exclusion Criteria
Mitral valve stenosis, prosthetic heart valve, active endocarditis, etc… Cardiac-Related
Conditions:
Hemorrhage
Risk-Related
Criteria:
Active internal bleeding, planned invasive procedure with potential for uncontrolled bleeding, including major surgery, platelet count
<90,000/μL, sustained uncontrolled hypertension, etc…
Concomitant
Conditions and
Therapies:
Severe, disabling stroke within 3 months or any stroke within 14 days before randomization, treatment with ASA >100mg daily, pregnant or breast-feeding, CrCl <30ml/min at screening, etc…
Study
Participation and
Follow-Up
Related Criteria:
Serious concomitant illness associated with life expectancy of less than 2 years, drug addiction or alcohol abuse within 3 years, have received experimental drug within 30 days, inability or unwillingness to comply with study-related procedures, etc…
Baseline Demographics:
Median age was 73 years
39.7% women; 60.3% male
90.5% of patients had hypertension
54.8% of patients had previous stroke or systemic embolism
62.4% of patients had previous use of warfarin
Baseline characteristics did not differ significantly between the two treatment groups.
14,264 patients were randomly assigned to receive:
Fixed-dose rivaroxaban 20 mg daily or 15 mg daily in patients with CrCl 30-49 mL/min
AND placebo (n = 7,131)
Dose-adjusted warfarin (target INR 2.0-3.0)
AND placebo (n = 7,133)
Patients were seen at weeks 1, 2, and 4, then monthly for duration of study to measure INR, primary endpoint events,
TIA, MI, medical/surgical procedures, adverse events and vital stats
Median duration of treatment: 590 days
Median follow-up period: 707 days
Primary
Endpoint
Composite of stroke (ischemic or hemorrhagic) and systemic embolism
Secondary
Endpoints
Safety
Endpoint
Composite of stroke, systemic embolism, or death from cardiovascular causes
Composite of stroke, systemic embolism, death from cardiovascular causes, or myocardial infarction
Individual components of the composite endpoints.
Composite of major and non-major clinically relevant bleeding events
Primary Analysis:
Performed in the per-protocol population
▪ Included all patients who received at least one dose of a study drug, did not have major protocol violation, and were followed for events while receiving drug or within 2 days after discontinuation.
Power of 95%
▪ 363 events needed; study used 405 events
One-sided significance level of 0.025
If noninferiority was achieved in the primary analysis,
Primary Superiority Analysis:
▪ Performed in the as-treated safety population
▪ Included patients who received at least one dose of a study drug and were followed for events, regardless of adherence to the protocol, while they were receiving the assigned study drug or within 2 days after discontinuation.
▪ Two-sided significance level of 0.05
▪ Key secondary endpoints were also tested for superiority in the as-treated safety population.
Testing for noninferiority and superiority was also performed in the intention-to-treat population
Included all patients who underwent randomization and were followed for events during treatment or after premature discontinuation
Hazard ratios, confidence intervals, and P values were calculated using Cox proportional-hazards models
Warfarin group:
Rosendaal method - calculate overall time that INR values fell within therapeutic range
Hazard Ratio (AKA Relative Risk or Risk
Ratio) :
The ratio of risk of an outcome event occurring in the experimental group compared to the risk of the same outcome event occurring in the control group.
HR < 1.0 indicates the therapy decreased the risk of developing the adverse outcome
HR = 1.0 indicates no difference between treatments
HR > 1.0 indicates the therapy increased the risk of developing the adverse outcome
NNT ( primary endpoint – stroke and systemic embolism
):
ARR = 241/7,004 – 188/6,958 = 0.0074
NNT = 1/0.0074 = 135
NNH ( safety endpoint – major and nonmajor bleeding
):
ARI = 1,475/7,111 – 1,449/7,125 = 0.004
NNH = 1/0.004 = 250
In patients with atrial fibrillation, rivaroxaban was noninferior to warfarin for the prevention of stroke or systemic embolism.
There was no significant difference in the risk of major bleeding between groups, although intracranial and fatal bleeding occurred less frequently in the rivaroxaban group.
LIMITATIONS
In warfarin group, INR values were within therapeutic range only 55% of the time.
Switching from per-protocol population to as-treated safety population to achieve superiority.
The primary endpoint of stroke was a composite of ischemic and hemorrhagic strokes.
No inclusion of data for increased GI bleeding
STRENGTHS
Randomized, double-blind, multi-center study with a large sample size
Treatment groups appeared similar at baseline
Included almost 40% females
Duke Clinical Research
Institute coordinated the trial, managed database, and performed primary analyses independently of the sponsors.
Rivaroxaban is a potential alternative to warfarin, especially for patients with compliance issues.
Things to consider:
Cost
No Antidote
Monitoring for coagulation parameters needed
How to bridge patients when switching from warfarin to rivaroxaban?
Long-term effects?
1.
2.
3.
Patel MR, et al. Rivaroxaban versus Warfarin in Nonvalvular Atrial
Fibrillation. New England Journal of Medicine. 2011; 365:883-891.
Supplement to: Patel MR, et al. Rivaroxaban versus Warfarin in
Nonvalvular Atrial Fibrillation. New England Journal of Medicine.
2011; 365:883-891. DOI: 10.1056/NEJMoa1009638.
Xarelto® (rivaroxaban) Product Package Insert. 2011; July. Janssen
Pharmaceuticals, Inc. Titusville, NJ.