SYB NOAC Policy - 16 October 2013
advertisement

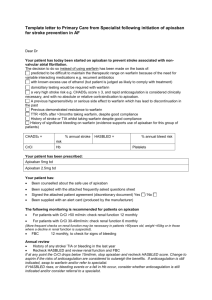
Strategic Clinical Networks and Senates Yorkshire and the Humber Yorkshire & the Humber Cardiovascular Strategic Clinical Network (South) SYCOM Policy Statement Non vitamin K antagonists for the prevention of stroke and transient ischaemic attack (TIA) in patients with non–valvular atrial fibrillation (AF) at increased risk of stroke. This paper represents the review of the initial NORCOM guidance for non-vitamin K antagonists agreed in June 2012. It is in line with experience gained from the first 12 months of using non vitamin K antagonists in non-valvular atrial fibrillation and the publication by NICE of three guidelines relating to non-vitamin K antagonists available as alternatives to warfarin to prevent stroke and TIA in patients with non–valvular AF (TA249 Dabigatran and TA256 Rivaroxaban and TA275 Apixaban). This paper outlines the consensus from a clinical advisory group formed to represent the relevant clinical specialties across the North Trent Cardiac and Stroke Network catchment for the express purpose of advising on the development of this treatment policy. Patients with atrial fibrillation with a CHADS2 score of 1 or more (or equivalent annual stroke risk ≥3%) should be offered an anticoagulant. In a primary care setting the proactive identification of patients with non-valvular AF at increased risk of stroke and not on an anticoagulant should be undertaken using audit tools such as GRASP-AF or via the QOF register. Patients identified to be in this group should be reviewed and the range of available options discussed. When deciding between agents safety considerations should be paramount. The non-vitamin K antagonists should be offered as an option as part of an informed discussion. Additional information is available to inform the discussion between doctor and patient. However prescribers may wish to be mindful of the following: The non-vitamin K antagonists are new drugs and do not have the long term safety record of warfarin; they are more expensive than warfarin; they may however offer substantial benefits to those unable to take warfarin. The balance of risk and benefit may favour non-vitamin K antagonists for patients presenting with TIA or minor stroke or stroke where rapid anticoagulation may further reduce the risk of subsequent strokes. Local formularies should decide the most appropriate Non -vitamin K antagonists for use locally Local decision makers are well placed to decide on the most appropriate agents to be used locally, using factors for example evidence base for outcomes and side effects, relative costs and experience of the agents. South Yorkshire & Bassetlaw NOAC Policy FINAL 16.10.13 Patients who are well controlled on warfarin (defined by a lack of poor control, below) should generally be maintained on warfarin. NICE states that for people already taking warfarin the potential risks and benefits of switching to a non-vitamin K antagonist should be considered in the light of their level of INR control. Patients who are currently prescribed warfarin with poor control, (defined as one INR above 8, or 2 readings outside the range of 1.8 to 5 in a six month period) should be considered for a non-vitamin K antagonist. These are the levels defined by local haematologists that are considered to increase the risk of bleeding or cardiovascular event to a degree where a change in agent would be appropriate. This approach will give wider access to for non-vitamin K antagonists and part of a managed introduction of these agents, building on experience in the first year of use. Increasing the access to these new drugs should enable more patients to be given primary and secondary prevention and further reduce the incidence of stroke. MHRA Guidance: For all the new oral anticoagulants the MHRA have issued guidance drawing attention to the risk factors for bleeding, the need to pay attention to posology, contraindications, and warnings and precautions for use to reduce the risk of bleeding. Available at: http://www.mhra.gov.uk/home/groups/plp/documents/drugsafetymessage/con321961.pdf References NICE Atrial fibrillation (CG36). Available at: http://guidance.nice.org.uk/CG36 NICE TA 249 Atrial fibrillation - dabigatran etexilate (TA249). Available at: http://guidance.nice.org.uk/TA249 NICE TA256 Rivaroxaban for the prevention of stroke and systemic embolism in people with atrial fibrillation. Available at: http://guidance.nice.org.uk/TA256 NICE TA275 Apixaban for preventing stroke and systemic embolism in people with nonvalvular atrial fibrillation. Available at http://guidance.nice.org.uk/TA275 This document should be read in conjunction with prescribing information found in the British National Formulary and Summary of Product Characteristics; prescribers should ensure they have the relevant information found in these sources prior to prescribing for non-vitamin K antagonists. This guidance should be reviewed following material change in the evidence base for nonvitamin K antagonists in atrial fibrillation or associated NICE guidelines. Richard Crosby NHS South Yorkshire and Bassetlaw Commissioning Support Unit On behalf of the SY&B Consensus Group of Clinical Specialists 8TH October 2013 South Yorkshire & Bassetlaw NOAC Policy FINAL 16.10.13 Appendix 1: Contra indications for warfarin and non vitamin K antagonists as specified in the summary of product characteristics (SPC) for each drug. Warfarin o o o o o o Known hypersensitivity to warfarin or to any of the excipients Haemorrhagic stroke Clinically significant bleeding Within 72 hours of major surgery with risk of severe bleeding Within 48 hours postpartum Pregnancy (first and third trimesters) Drugs where interactions may lead to a significantly increased risk of bleeding Rivaroxaban o o o o o Hypersensitivity to the active substance or to any of the excipients Active clinically significant bleeding. Lesion or condition, if considered to be a significant risk for major bleeding. This may include current or recent gastrointestinal ulceration, presence of malignant neoplasms at high risk of bleeding, recent brain or spinal injury, recent brain, spinal or ophthalmic surgery, recent intracranial haemorrhage, known or suspected oesophageal varices, arteriovenous malformations, vascular aneurysms or major intraspinal or intracerebral vascular abnormalities. Concomitant treatment with any other anticoagulants e.g. unfractionated heparin (UFH), low molecular weight heparins (enoxaparin, dalteparin, etc.), heparin derivatives (fondaparinux, etc.), oral anticoagulants (warfarin, , dabigatran etexilate, apixaban etc.) except under the circumstances of switching therapy to or from rivaroxaban or when UFH is given at doses necessary to maintain an open central venous or arterial catheter. Hepatic disease associated with coagulopathy and clinically relevant bleeding risk including cirrhotic patients with Child Pugh B and C Pregnancy and breast feeding Dabigatran o Hypersensitivity to the active substance or to any of the excipients o Patients with severe renal impairment (CrCL < 30 mL/min) o Active clinically significant bleeding o Lesion or condition, if considered a significant risk factor for major bleeding. This may include current or recent gastrointestinal ulceration, presence of malignant neoplasms at high risk of bleeding, recent brain or spinal injury, recent brain, spinal or ophthalmic surgery, recent intracranial haemorrhage, known or suspected oesophageal varices, arteriovenous malformations, vascular aneurysms or major intraspinal or intracerebral vascular abnormalities o Concomitant treatment with any other anticoagulants e.g. unfractionated heparin (UFH), low molecular weight heparins (enoxaparin, dalteparin etc), heparin derivatives (fondaparinux etc), oral anticoagulants (warfarin, rivaroxaban, apixaban etc) except under the circumstances of switching therapy to or from Pradaxa or when UFH is given at doses necessary to maintain an open central venous or arterial catheter o Hepatic impairment or liver disease expected to have any impact on survival o Concomitant treatment with systemic ketoconazole, cyclosporine, itraconazole, tacrolimus and dronedarone o Prosthetic heart valves requiring anticoagulant treatment Apixaban o o o o o Hypersensitivity to the active substance or to any of the excipients Active clinically significant bleeding. Hepatic disease associated with coagulopathy and clinically relevant bleeding risk Lesion or condition if considered a significant risk factor for major bleeding. This may include current or recent gastrointestinal ulceration, presence of malignant neoplasms at high risk of bleeding, recent brain or spinal injury, recent brain, spinal or ophthalmic surgery, recent intracranial haemorrhage, known or suspected oesophageal varices, arteriovenous malformations, vascular aneurysms or major intraspinal or intracerebral vascular abnormalities. Concomitant treatment with any other anticoagulant agent e.g. unfractionated heparin (UFH), low molecular weight heparins (enoxaparin, dalteparin, etc.), heparin derivatives (fondaparinux, etc.), oral anticoagulants (warfarin, rivaroxaban, dabigatran, etc.) except under the circumstances of switching therapy to or from apixaban or when UFH is given at doses necessary to maintain an open central venous or arterial catheter *http://www.gpnotebook.co.uk/simplepage.cfm?ID=x20030129224615665170 This table should be read in conjunction with the SPC for each drug available at http://www.medicines.org.uk/EMC/default.aspx Clinicians should use their clinical judgement where cautions rather than contraindications are listed in the SPC as to the risks vs. the benefits of starting a particular and ensuring appropriate monitoring is carried out if required. South Yorkshire & Bassetlaw NOAC Policy FINAL 16.10.13