Board Exams CRT and RRT - Respiratory Therapy Files
advertisement
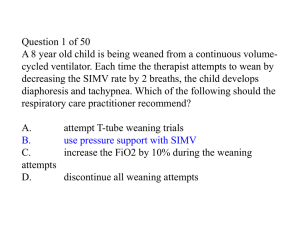
Board Exam Preparation Written Exams CRT and RRT Be Prepared! WHAT to study WHERE to study WHEN to study HOW to study What to Study Know Your Enemy: The Board Exams You must understand the structure and content of the board exams and apply this knowledge to your study plan. REVIEW THE MATRIX FOR THE CRT, RRT, CSE ALL FOUND ON WWW.NBRC.ORG The EXAM Part one: Study all content, take plenty of practice exams, schedule your CRT exam and layout a study plan After completing the CRT schedule your Written RRT and Clinical Simulation exam. You may take both the same day or seperate Exam Structure CRT 160 questions 140 actual test questions 20 additional questions that are NOT scored 3 hours Passing score 75% (105 correct)* RRT Written 115 questions 100 actual test questions 15 additional questions that are NOT scored 2 hours Passing score 70% (70 correct)* •Computer based testing •No calculators allowed •A pencil and paper will be provided for you Exam Structure CSE (Clinical Simulation Exam) PART 2 of the RRT Consists of 11 scenarios (only 10 are graded) Covers all areas from the CRT and WRRT Typically you will get disease management scenarios for: COPD, Trauma, Cardiovascular disease, Neuromuscular, Peds, Neonates, and others (page 450) Exam Content Content Outline Candidate Handbook www.nbrc.org All items on the exam are developed from these outlines Categorized by cognitive level Recall Application Analysis Recall: the ability to recall or recognize specific information Facts Definitions Normal values Principles Equations… Recall Involves remembering memorized information You either know it or you don’t If you don’t know the answer, eliminate answers that you think are impossible, and then guess from the remaining options. Recall Example An otherwise healthy 25-year-old male patient who took an overdose of sedatives is being supported on a ventilator. Which of the following measures of total static compliance would you expect in this patient? A. B. C. D. 100 mL/cmH2O 10 mL/cmH2O 1 mL/cmH2O 0.1 mL/cmH2O Answer A To evaluate and monitor a patient, you need to know what is normal and what is abnormal. This item tests your ability to recall normal static compliance. It also separately assesses your ability to differentiate the common bedside units used for this measure (mL/cmH2O) from that typically employed in a pulmonary lab (L/cmH2O). Application: the ability to comprehend or apply knowledge to new or changing conditions Tests your understanding of principles, practices, and procedures involved in respiratory care Application Example An adult patient receiving volume-oriented assist/control ventilation has a corrected tidal volume of 700 mL, a peak pressure of 50 cmH2O, and a plateau pressure of 40 cmH2O and is receiving 5 cmH2O of PEEP. What is the patient’s static compliance? A. B. C. D. 200 mL/cmH2O 20 mL/cmH2O 2 mL/cmH2O 0.2 mL/cmH2O Answer B This item tests your ability to apply a formula to a clinical situation (most formula-type questions are at the application level). To answer it correctly, you need to “plug” the correct data into the formula for computing static compliance Vt/(Ppl-PEEP) Analysis: the ability to analyze information, to put information together to arrive at solutions, and/or to evaluate the usefulness of the solutions They begin the question with facts that you need to analyze and interpret to come to a conclusion. They may ask what is wrong, or they may ask what do you want to do about it. Analysis: 10% of the exam. analyze or interpret information in order to solve a problem. Analysis Example A patient is receiving volume cycled mechanical ventilation in the control mode. The following ABG data were obtained:pH 7.56, PaCO2 25 torr, PaO2 93 torr, HCO3- 22 mEq/L Which ventilator adjustments should be made at this time? A. Institute 5 cmH20 PEEP B. Increase the FiO2 C. Increase the tidal volume D. Decrease the ventilatory rate Answer D This item assesses your ability to analyze monitoring data and apply this information to recommend a treatment approach for this patient. First, youmust analyze the data, which should reveal that the patient has uncompensated respiratory alkalosis. Second, you need to recognize that this can be due to overventilation. Last, you need to apply this data and your knowledge of mechanical ventilation to recommend the correct course of action The “NBRC Hospital” Treat the exam matrix as the policy manual for the NBRC hospital Focus on the things that you do not typically do at your clinic site As you study, identify things that are different that what you typically do Do not be afraid to use your independent judgement. The “NBRC Hospital” • You “enter” the NBRC hospital every time you take an NBRC exam. • This hospital may or may not function the same as the clinical site or sites you are at, it represents an idealized institution. • The NBRC RC department always relies of generally accepted knowledge based on various practice guidelines • Their “procedure manual” is based upon broad national agreement among clinicians and educators as to what common skills the average therapist performs • So upon entering the NBRC hospital, you may be expected to know and do different things from those you were trained to do. Your Textbook Bold Topic Headings Evaluate the patient’s general appearance (Code: IB1a) [Difficulty: ELE: R, Ap; WRE: An) The code refers to a section of the matrix ELE: entry level exam WRE: written registry exam R: recall, Ap: Application, An: Analysis Your Text Book Read xv through xxi For every chapter take the pre-test (answers and explanations are at the end of each chapter) and review the content areas specific for the exam Use the Jones and Bartlett Learning companion website REVIEW THE TEST TAKING TIPS AND TECHNIQUES APPENDIX page 511 Where and When to Study Choose a quiet, distraction free environment Establish and follow a strict study schedule How to Study Prepare yourself mentally and physically Be organized Organize your resources Create a “battle plan” Create a list of problem areas to focus on Use reflections to help with this! Get psyched! Create and maintain a positive attitude toward test preparation and test taking http://dus.psu.edu/academicsuccess/studyskills.html Test Taking Tips Pace yourself So that you have time to get through all questions “bookmark” questions Do not leave any blanks Completely read each question Determine what you are really being asked Test Taking Tips cont. Separate the important information From that which is not important Do not read beyond the question Use only what is given to you Carefully read each answer Pick the best answer offered Even if you don’t like it Test Taking Tips cont. Multiple multiples 1. Find an option that you know is incorrect and cross off any of the answers that contain it 2. Find an option that you know to be correct and cross off any answers that do not contain it 3. Find the remaining answer Test Taking Tips cont. Again, answer every question Take practice exams Evaluate your strengths and weaknesses Use reflection to help with this! Spend time studying your weak areas Maximize Exam Prep Time Spend the Majority of your time studying the most heavily tested areas: Mechanical Ventilation of the Adult Patient Assessment Bedside and Advanced Arterial Blood Gases Oxygen and Medical Gas Therapy Pharmacology Airway Management Maximize Exam Prep Time cont. Review the exam hints in all chapters ABG interpretation is a must! In order to answer mechanical ventilation and oxygen therapy questions Mechanical ventilation of the adult is the most heavily questioned content. You MUST understand mechanical ventilation to do well on the exams Taking the Test! Know What to Expect When Reporting to the Testing Center Arrive early Relax before the exam If you are more than 15 minutes late you will have to reschedule Bring two forms of ID You may only bring your wallet and keys into the testing center You will be provided with a pencil and scratch paper Know What to Expect There will be a short practice test Once you begin, you cannot ask questions You are allowed to take breaks Break time counts against your exam time Take the practice tests on-line at www.nbrc.org During the Test Get comfortable Answer all questions Budget your time Monitor your pace Answer easy questions first Bookmark difficult item and return to them later Use all the available time Test Preparation “… the most valuable resource you possess is your own ability and determination to succeed.” Malley, W., Clinical Blood Gases: Application and Noninvasive Alternatives, W.B. Saunders Co., Philadelphia, PA, 1990. Elements of an NBRC Multiple-Choice Question Scenario: Brief description of the clinical situation Stem: The statement that asks the question or specifies the problem Options: Possible answers to the question or solutions to the problem Keyed response: The correct answer Distracters: Wrong answers An 80 kg adult male patient with aspiration pneumonia receiving volume-oriented SIMV has the following ventilator settings and blood gas results: Mode SIMV Vt 500 mL Rate 12 FiO2 0.50 PEEP 5 cmH2O pH 7.29 PaCO2 52 mmHg HCO3- 25 mEq/L PaO2 63 mmHg SaO2 91% The respiratory therapist should do which of the following first? A. Increase the FiO2 B. Increase the tidal volume C. Add pressure support D. Increase PEEP The Scenario • Briefly describes a clinical situation that you need to assess. • Thoroughly review the scenario before even looking at the stem or options • Sometimes the scenario and stem are combined and must be reviewed together • Look for the following critical information • Look for the following information: • The location or setting (ICU, outpatient clinic, patient’s home) • The available resources (equipment being used or at hand) • Ventilator capable of volume SIMV • The patient’s general characteristics (age, size, disease process, mental status) • Adult, male, 80kg, aspiration pneumonia • Relevant objective data (ABG, PFT…) The Stem • Asks the question or directs your attention. • Often contains key words or phrases that may help you choose the correct answer • Priority: first, initially, best, priority, safest, most, least • Put a value on each option and place them in rank order • Sequence: before, after, next • Apply procedural knowledge or logic to place options in proper sequence • Absolutes: always, never • Find the only option that would be correct in every case every time The Stem • Negative polarity: not, except, contraindicated, unacceptable, avoid • Switch from being concerned with what is correct or true to what is false • Verbal associations: word or phrase in the stem that is identical or similar to a word in the correct answer • Select the option that includes wording similar to that found in the stem • What is the key word in the sample question? • First • A priority clue directing you to choose the action most immediately needed • The primary/most severe problem is respiratory acidosis • Keyed option B increase tidal volume The Stem Do not overanalyze! The simplest interpretation is generally the correct one. Anticipate the answer Before looking at the options available Options Every question has 4 options The Stem Stem Wording A Which of the following assessment procedures would help determine proper positioning of an endotracheal tube in the patient’s trachea? Stem Wording B Which of the following assessment procedures would help confirm proper positioning of an endotracheal tube in the patient’s trachea? • A tiny variation in wording makes a huge difference • A: breath sounds, capnography, tube insertion length, esophageal detection device, CXR… • B: CXR • Do not overanalyze! • The simplest interpretation is generally the correct one. • Anticipate the answer • Before looking at the options available Options Every question has 4 options When you are sure of the correct response, select it and move on Do not panic when you encounter questions that appear difficult or unfamiliar to you • • • All exam candidates encounter dozens of these questions Instead of getting flustered, get resourceful and use some of the following option selection strategies • Always look for the best option not just the correct one • Two or more options may be correct but one likely is most correct in the particular circumstances or with the specific patient described • When you are unsure of the correct option, switch from finding the right answer to finding the wrong answer(s) • Eliminate options you know to be incorrect; each time you eliminate a distracter, you increase your chances of answering the question correctly • When in doubt, give each option a “true-false” test as compared with the stem (the true statement is usually the best answer) • Be wary of options that are totally unfamiliar to you; more often than not unfamiliar options are distracters • If you encounter a “double negative” in a stem and option, remember that it creates the equivalent positive statement • Avoid impulsively selecting an option simply because it provides correct information as an option can provide correct information but still be the wrong choice because it does not answer the question asked Let’s look at some more specific strategies… Which of the following is true regarding patients in the early stages of an asthmatic attack? A. They all exhibit respiratory alkalosis B. They always have moderate hypoxemia C. They have decreased expiratory flows D. They never respond to beta adrenergics • • • • • • • Absolutes Correct answer: C Always, never, all, every, none, only These key words indicate that the option has no exceptions More often than not, options that use absolutes are false Generally you should avoid choosing an option that must be true or false every time without exception You do not see this very frequently in the board exams Some absolutes , especially this efounded in rules or standards, may be a correct option • “ you must always properly identify the patient before treatment” holds without exception A patient’s advance directive: A. Is usually obtained at the time of admission B. Can be found in the doctor’s progress notes C. Represents a guideline, not a legal requirement D. Cannot be altered after it is written and signed • • • Qualifiers Correct answer A A qualifier is the opposite of an absolute Usually, probably, often, generally, may, frequently, seldom • Options that contain qualifiers usually represent good choices • The NBRC minimizes its use of qualilfiers An intubated patient is receiving volume control ventilation. The patient’s condition has not changed, but you observe higher peak inspiratory pressures than before. Which of the following is t he most likely cause of this problem? A. There is a leak in the patient-ventilator system B. The endotracheal tube cuff is deflated C. The endotracheal tube is partially obstructed D. The endotracheal tube is displaced into the pharynx Equally Plausible Options • Correct answer C • You will often see question that contain two options that are very similar to equivalent to each other • Options A and B are equivalent because they both represent a leak in the system • Usually when two items are very similar or equivalent, they are distracters and should be eliminated Over a 3 hour period, you note that a patient’s plateau pressure has remained stable, but her peak pressure has been steadily increasing. Which of the following is the best explanation for this observation? A. The patient’s airway resistance has increased B. The patient is developing atelectasis C. The patient’s compliance has decreased D. The patient is developing pulmonary edema Equally Plausible Options • Correct answer A • B,C, and D all represent decreases in compliance thus are equivalent • The “odd man out” is the correct answer You are assisting with the oral intubation of an adult patient. After the ET tube has been placed, you note that breath sounds are decreased on the left compared with the right lung. What is the most likely cause of this? A. The tip of the tube is in the right mainstem bronchus B. The cuff of the endotracheal tube has been overinflated C. The endotracheal tube has been inserted into the esophagus D. The tip of the tube is in the left mainstem bronchus Opposite Options • Correct answer A • In general, when you encounter two options that are opposites, chances are the correct choice is one of the two • A and D are opposites, one of them is most likely the correct answer • There are exceptions to this strategy A patient receiving long-term positivepressure ventilatory support exhibits a progressive weight gain and a reduction in the hematocrit. Which of the following is the most likely cause if this problem? A. Leukocytosis B. Chronic hypoxemia C. Water retention D. Leukocytopenia Opposite Options • Correct answer C • A and D are opposites but in this case they are distractors In reviewing the PFT results of a 67-yearold smoker with an admitting diagnosis of emphysema and chronic bronchitis, you would expect which of the following general findings? A. Increased airway resistance and decreased lung compliance B. Increased airway resistance and increased lung compliance C. Decreased airway resistance and decreased lung compliance D. Decreased airway resistance and increased lung compliance Duplicate Facts in Options • Correct answer B • This question’s options contain two contrasting statements: increased/decreased resistance and increased/decreased compliance. • Identify any statement that you know is either true or false. • If you know that patients with emphysema and chronic bronchitis typically have increased airway resistance you can eliminate options C and D. When instructing a patient how to breathe during a small-volume nebulizer drug treatment, the respiratory therapist coaches the patient to hold his breath at the end of inspiration. The purpose of this maneuver is to improve: A. Drug delivery B. Particle stability C. Aerosol penetration D. Inertial impaction • • • Global Options Correct answer A A is the most general or global alternative B, C, and D are all factors that fall under the broader concept of enhanced drug delivery, making option A the best choice. You obtain an SpO2 measurement on a patient of 80%. Assuming this is an accurate measure of hemoglobin saturation, what is the patient’s approximate PaO2? A. 40 torr B. 50 torr C. 60 torr D. 70 torr Options Constituting a Range • Correct answer B • Item writers often try to mask the correct choice by placing it within a set of higher and lower values. • Consider eliminating the highest and lowest values and choosing an option in the middle. • “40-50-60/70-80-90” A portable spirometer requires that you enter the patient’s height in centimeters in order to derive normal values. The patient tells you that she is 5 feet 6 inches tall. What value would you enter into the device? A. 26 cm B. 66 cm C. 168 cm D. 186 cm • • • Math Problems Correct answer C 66 in x 2.54 Or approximately 2 x 66 + ½ 66 = 66+66+33 = 168 • 66/2.54 = 26 answer choice A is a good distracter • Use scratch paper • Ste up the problem properly • Try estimating the answer without calculating • Do your computation twice to confirm the answer • Many distracters are based on common formula or computation errors, do not immediately select an answer that matches your calculation • If you absolutely do not know choose from the answers in the middle During postural drainage of the left lower lobe, a patient complains of acute chest pain. Which of the following would you do? A. Give the patient supplemental oxygen B. Continue the treatment with the bed flat C. Ask the nurse to administer pain medication D. Discontinue the treatment and monitor the patient The Triple S Rule • Correct answer D • If a patient gets worse while you are giving therapy… • Stop, stabilize, stay • Stop what you are doing • Stabilize the patient • Stay with the patient A 45-year-old patient with asthma is prescribed 0.3 mL of albuterol (Proventil) in 3 mL normal saline via small-volume nebulizer. Before initiating therapy, you note from chart review that the patient is severely hypertensive and has been experiencing episodes of supraventricular tachycardia. You should do which of the following? A. Administer the treatment as ordered B. Postpone the treatment and notify the physician C. Dilute the albuterol with extra normal saline D. Decrease the amount of albuterol administered The Triple S Rule (part 2) • Correct answer B • A corollary to the triple S rule is to never start therapy if the patient is exhibiting abnormal signs ir symptoms that could be worsened by your action A patient is admitted to the emergency department comatose with suspected smoke inhalation. After confirming airway patency, which of the following should you do first? A. Measure the SpO2 B. Initiate 100% Oxygen C. Obtain an arterial blood gas D. Request a STAT chest X-ray Act First, Ask Questions Later • Correct answer B • Obtaining additional information is important but given that the patient is suspected of smoke inhalation 100% oxygen should be administered immediately You are called to the bedside of a patient by her ICU nurse to check the attached volume ventilator. You note that both the low-volume and high-pressure limit alarms are sounding on each breath, Your first action should be to: A. Disconnect patient and manually ventilate with 100% oxygen B. Call the attending physician for further patient information C. Check the patient’s chart for the original ventilator orders D. Ask the nurse about how recently the patient was suctioned Act First, Ask Questions Later • Correct answer A • B,C, and D nay help you evaluate the problem but they waste precious time. • Your priority os patient safety A 60-kg (132-lb) COPD patient is receiving SIMV with a Vt of 500 mL at a rate of 9/min with an FiO2 of 0.35. Blood gases are as follows: pH = 7.36; PaCO2 = 61 torr; HCO3- = 36 mEq/L; PaO2 = 64 torr. Which of the following changes would you recommend at this time? A. Increase the IMV rate B. Increase the FiO2 C. Maintain settings D. Increase the Vt If It Ain’t Broke, Don’t Fix It! • Correct answer C A 30-kg (66-lb) child is being mechanically ventilated in the SIMV mode. The following data are available: Ventilator settings: FiO2 0.45; mandatory rate 18; total rate 23; Vt 350 mL; PEEP 12 cmH2O. Blood gases: pH 7.38; PaCO2 42 toor; PaO2 110 torr; HCO3- 23 mEq/L, BE 0 mEq/L. Based on these data, which of the following should you do? A. Decrease the tidal volume B. Reduce the PEEP C. Decrease the rate D. Lower the FiO2 Back Off Bad! • Correct answer B The following data are available for a patient: Blood Gas Analyzer Co-Oximeter pH 7.35 OxyHb 97% PaCO2 28 torr CarboxyHb 1% HCO3- 14 mEq/L MetHb 1% BE -10 mEq/L Hb 18.8 g/dl PaO2 40 torr SaO2 73% You should do which of the following? A. Report the SaO2 value at 73% B. Report the SaO2 value as 97% C. Recommend administration of bicarbonate D. Recalibrate the instruments and repeat the analysis Data Just Don’t Jive • Correct answer D • Large discrepancy between PaO2, SaO2 and OxyHb The results of an arterial blood gas analysis for a patient who is breathing 100% oxygen are below: pH 7.27; PaCo2 44 torr; HCO3- 23 mEq/L; BE +1; PaO2 598 torr; SaO2 100%. Which of the following is the likely problem? A. Respiratory acidosis B. Large physiologic shunt C. Metabolic acidosis D. Laboratory error Errors, Errors, Everywhere! • Correct answer D • When ever you have laboratory error as an option, always check the numbers • PaO2 is normal (use alveolar air equation) • Acid base status is impossible based on theHenderson-Hasselbach equation A doctor asks you to assess if a 75-kg (165-lb) patient with a neuromuscular disorder being mechanically ventilated in the SIMV mode is ready for weaning. You obtain the following data during a bedside ventilatory assessment: spontaneous Vt 250 mL; Minute ventilation 10 L/min; Vital Capacity 750 mL; MIP -28 cm2O. Based on thus information, which of the following would you recommend? A. Begin a spontaneous breathing T-piece trial B. Postpone weaning and reevaluate the patient C. Begin weaning using a pressure support protocol D. Begin weaning by decreasing the SIMV rate Don’t Know What You’re Missing! Correct answer B VC and MIP are borderline adequate But Vt and VE suggest a major problem Spontaneous rate = 10 L/min / 250 mL/breath = 40 breaths/ minute • RSBI = 40/0.25 – 160 • Review the numbers to see what is missing! • • • • A surgeon orders an increase in PEEP from 6 to 10 cmH2O for a post-op patient receiving mechanical ventilation. After you adjust the PEEP setting, you note a rapid fall in the patient’s arterial blood pressure and a rapid rise in her heart rate. Which of the following actions would you recommend to the surgeon? A. Increase the FiO2 by 10% B. Administer a vasopressor C. Return The PEEP to 6 cmH2O D. Obtain a STAT blood gas Jump Back, Jack! • Correct answer C • When things go bad, many times your action immediately preceded things going bad • The best course of action is the reverse course and undo what you have just done • One of the adverse effects of PEEP is decreased cardiac output • Due to increased pleural pressure and decreased venous return Manual ventilation of a patient with a selfinflating bag-valve-mask device fails to inflate the patient’s chest adequately. You should do which of the following? A. Intubate and mechanically ventilate the patient B. Switch to a gas-powered resuscitator with mask C. Reposition the patient’s head, neck, and mask D. Insert a laryngeal mask airway (LMA) KISS It! • Correct answer C • The simplest and should be tried before moving on to more aggressive options When checking a ventilator, you discover that the set PEEP level cannot be maintained. Which of the following might be causing this problem? I. Leak in the tubing II. Faulty exhalation valve III. Leak around the airway cuff IV. Loose humidifier connection A. I and II B. I and III C. II and IV D. I, II, III, and IV Gas Goes In, Gas Comes Out • Correct answer D • You will be asked questions that ask you to differentiate between a leak and an obstruction • Leaks prevent pressure buildup • Obstructions cause pressure buildup At the bedside of a patient receiving volume-oriented mechanical ventilation, you suddenly observe that simultaneous sounding of the high-pressure and lowvolume alarms. Which of the following is the most likely cause of this problem? A. A leak in the ET tube cuff B. A mucous plug in the ET tube C. Ventilator circuit disconnection D. Development of pulmonary edema Gas Goes In, Gas Comes Out • Correct answer B • Obstructions can be more difficult to identify because they can either be partial or complete • High pressure/low volume = obstruction • Low pressure/low volume = leak • B and D both cause obstruction but the one that would arise suddenly is the mucus plug Which of the following would facilitate clearance of pulmonary secretions in a patient with cystic fibrosis? I. Mucomyst II. Flutter valve III. Atropiene IV. DNase A. I and III B. II and IV C. I, II, and IV D. II, III, and IV Love Those Multiple Multiples! • Correct answer C During a short pause from resuscitation of a child in the emergency department, you cannot palpate a carotid pulse but observe the following rhythm on the ECG monitor (next slide) Which of the following actions should you take at this time? A. Resume cardiac compressions and ventilation B. Discontinue compressions and monitor the patient C. Recommend cardioversion at 100 Joules D. Recommend epinephrine administration Treat the Patient, Not the Monitor! • Correct answer A • They will give you scenarios where the patient and monitor data conflict • Pulse oximetry data • ECG • PEA • Remember the ECG only represents electrical activity and a patient with no pulse requires resuscitation A physician has ordered albuterol (Proventil) and deoxyribonuclease (DNase) by aerosol for a cystic fibrosis patient who also receives postural drainage 3 times a day. You should administer these therapies in which of the following sequences? A. DNase, postural drainage, albuterol B. Albuterol, DNase, postural drainage C. Postural drainage, albuterol, DNase D. DNase, albuterol, postural drainage • • • • Keeping Order Correct answer B Open ‘em up Thin ‘em down Clear ‘em out A 90-kg (198-lb) patient is being ventilated in the postanesthesia care unit (PACU) following upper abdominal surgery. Ventilator settings and arterial blood gas date are as follows: Ventilator Settings: Blood Gases: Mode SIMV pH 7.51 Vt 800 mL PaCO2 31 torr Set rate 14/min HCO3- 24 mEq/L Total rate 14/min BE +1 FiO2 0.40 PaO2 115 torr PEEP 5 cmH2O SaO2 99% You should recommend which of the following? A. Increase the FiO2 B. Decrease the rate C. Decrease the tidal volume D. Discontinue PEEP Give me a V; Give me an O! • Correct answer B • You must be able to interpret blood gases • You must be able to differentiate between an ventilation problem versus an oxygenation problem A 45-year-old 70-kg (154-lb) male with a diagnosis of bilateral pneumonia is receiving volume-controlled ventilation in the SIMV mode. Ventilator settings and blood gas data are below: Ventilator Settings: Blood Gases: Mode SIMV pH 7.35 Vt 700 mL PaCO2 345 torr Set rate 6/min HCO3- 23 mEq/L Total rate 10/min BE -1 FiO2 0.65 PaO2 55 torr PEEP 5 cmH2O SaO2 83% Which of the following shoud be recommended? A. Increase PEEP B. Increase the rate C. Increase the FiO2 D. Add an inspiratory plateau Give Me a V; Give Me an O! • Correct answer A • Hypoxemia is present so both A and C would help • Use the 60/60 rule • PaO2 > 60 & FiO2 < 0.60 maldistribution of ventilation = increase FiO2 • PaO2 < 60 & FiO2 > 0.60 physiologic shunting = add/increase PEEP/CPAP A nurse tells you that his patient is scheduled to start chest physiotherapy four times a day this morning and that he would like you to get started before she goes to radiology for a CT scan. Which of the following should you do first? A. Auscultate and percuss the patient’s chest B. Initiate therapy after reviewing the X-ray C. Interview the patient to obtain a history D. Confirm the doctor’s order in the chart Who’s in Charge Here? • Correct answer D GOOD LUCK! Resources Scanlan et. Al. Certified Respiratory Therapist Exam Review Guide. 2010. Jones and Bartlett.