Otitis Media - RahulGladwin.com
advertisement
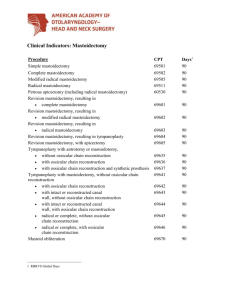
Childhood Otitis Media By Rahul Gladwin, MS3 University of Health Sciences Antigua School of Medicine Email: rahul[AT]rahulgladwin.com Otitis Media definition Otitis Media is defined as an inflammation of the middle ear i.e., the area between the tympanic membrane and the inner ear. Pathogenesis Infection mostly occurs in infants and children because of the shorter and more horizontal orientation of the Eustachian tube which allows reflux from the pharynx. Bacterial Etiology S. pneumonia. 1. Incidence: 38% 2. Beta Lactamase producing: 15-25% 3. Causes more severe cases with Otalgia and fever. Nontypeable H. influenzae. 1. Incidence: 27% 2. Beta Lactamase producing: 35% 3. More often associated with eye redness and discharge. Moraxella catarrhalis. 1. Incidence: 10% 2. Beta Lactamase producing: 85-100% Viral Etiology 57% 35% 33% 30% 28% 18% 10% of of of of of of of RSV, influenza A, parainfluenza type 3, adenovirus, parainfluenza type 1, influenza B and parainfluenza type 2 virus infections. Fungal Etiology Aspergillus or Candida Correlation factors Signs Crying, Irritability, Tugging or pulling on the ear. Symptoms Ear pain, Rhinitis, Cough, Ear drainage, Hearing loss, Fever. Complications Acute mastoiditis – infection of the mastoid process. Cholesteatoma – cystic lesion within the middle ear. Meningitis. Hearling loss. Tympanic membrane perforation. Brain abscess. Ear Anatomy Ear Anatomy Types of Otitis Media Acute Otitis Media Most common type seen in children Occurs when there is fluid in the middle ear Occurs with inflammation of the TM May be bacterial or viral Phases of Acute Otitis Media 1st phase - exudative inflammation lasting 1–2 days, fever, rigors, meningism (occasionally in children), severe pain (worse at night), muffled noise in ear, deafness, sensitive mastoid process, ringing in ears (tinnitus) 2nd phase - resistance and demarcation lasting 3–8 days. Pus and middle ear exudate discharge spontaneously and afterwards pain and fever begin to decrease. This phase can be shortened with topical therapy. 3rd phase - healing phase lasting 2–4 weeks. Aural discharge dries up and hearing becomes normal. Types of Acute Otitis Media Otitis Media without effusion Inflammation of the TM with fluid in the middle ear May cause myringitis (cyst on TM) Present during the beginning stages of otitis media Formation of painful blisters on the eardrum (tympanum). Types of Acute Otitis Media Serous Otitis Media or Otitis Media with effusion Inflammation of the TM with fluid in the middle ear Caused by vacuum created by malfunction of the Eustachian tube Can cause hearing impairment and delayed speech in children Since infants cannot hear they cannot learn how to talk Chronic Otitis Media Occurs when the middle ear infection perists and causes significant hearing loss and damage to the middle ear May involve a perforation of the TM Pus may drain through the ear canal – a concept called otorrhea Chronic Otitis Media - Types Tubotympanic disease – called safe disease. The infection is limited to the mucosa and the antero inferior part of the middle ear cleft, hence the name. This disease does not have any risk of bone erosion. Atticoantral disease – called unsafe disease. Fatal intra-cranial and extra-cranial complications can occur. Disease spreads by erosion of the bony wall of the attic. Cholesteatoma may occur. Commonly seen in sclerosed mastoid cavities. Recommended Otitis Media Workup Laboratory Studies – sepsis workup Imaging - study of choice is a contrastenhanced CT scan of the temporal bones MRI is more helpful in depicting fluid collections Tympanometry may help with diagnosis in patients with OM with effusion Diagnostic criteria for OM Bulging TM Retracted TM Impaired mobility of the TM Loss of light reflex Erythematous TM Purulent otorrhea Opacification of the TM Normal TM Appears as: Glistening, translucent (scarring often may be evident in adults). Light reflex extending anteriorly/inferiorly from the umbo (most depressed part of the tympanic membrane). Pearly gray to pale pink membrane with cone of light well visualized. Mobile (to the air pulses). Non-erythematous. Handle (manubrium) and short process of malleus well identified. Normal Right TM Acute Otitis Media-TM Acute Otitis Media Serous Otitis Media Serous Otitis Media Ruptured TM Ruptured TM Otorrhea Myringitis - blisters on TM Myringitis - blisters on TM Cholesteatoma Cholesteatoma Brain Abscess Mastoiditis Mastoiditis Otitis Media Pathology Video http://www.youtube.com/watch?v=1km sPEd2Efk&feature=related Quick Statistics More common in Caucasian children. 70% of all children have at least 3 infections before the age of 6. Children given antibiotics were 2-6 more likely to get re-infected. About 2 to 3 out of every 1,000 children in the United States are born deaf or hard-of-hearing. Nine out of every 10 children who are born deaf are born to parents who can hear. Approximately 188,000 people worldwide have received cochlear implants. In the United States, roughly 41,500 adults and 25,500 children have received them. Trends on newborn screening Office visits for OM Treatment with penicillin 1. Antibiotic duration 1. Age under 6 years 2. First Line 1. Amoxicillin 80-90 mg/kg/day PO divided twice daily for 10 days (7 days if age>6) 2. If Penicillin Allergy, use Macrolide (e.g. Azithromycin) 3. Second Line (10 day course) 1. Amoxicillin with clavulanate (Augmentin) 90 mg/kg/day divided twice daily for 10 days 2. Cefuroxime (Zinacef, Ceftin) 30 mg/kg/day divided twice daily for 10 days 3. Cefprozil (Cefzil) 30 mg/kg/day divided twice daily for 10 days 4. Cefdinir (Omnicef) 14 mg/kg/day divided one to two times daily fo 10 days 5. Cefpodoxime (Vantin) 30 mg/kg once daily for 10 days 4. Third Line 1. Strongly consider Tympanocentesis for bacterial culture 2. Ceftriaxone (Rocephin) 50 mg/kg IM daily for 3 days 3. Clindamycin 30-40 mg/kg/day divided four times daily for 10 days. Treatment if allergic to penicillin 1. Consider Tympanocentesis 2. Clindamycin (Cleocin) 30-40 mg/kg/day (max 1800 mg) divided four times daily for 10 days 3. Macrolide antibiotics (High bacterial resistance rate) 1. Erythromycin 2. Clarithromycin (Biaxin) 15 mg/kg/day divided twice daily for 10 days 3. Azithromycin (Zithromax) 1. One dose of Azithromycin XR (Zmax) at 30 mg/kg (up to 1500 mg) or 2. Three days of Azithromycin at 20 mg/kg/day once daily (up to 500 mg/day) or 1. This high dose approached Augmentin efficacy in one study 2. Arrieta (2003) Antimicrob Agents Chemother 47:3179 3. Azithromycin 10 mg/kg (max: 500 mg) day 1, then 5 mg/kg/day (max 250 mg) for 5 days 4. Fluoroquinolones (avoid under age 16 years) 1. Gatifloxacin (Tequin) 2. Levofloxacin (Levaquin) 3. Moxifloxacin (Avelox) Resources Robbins Pathology Kaplan CK Lecture notes www.fpnotebook.com www.ncbi.nlm.nih.gov www.nidcd.nih.gov www.medicinenet.com emedicine.medscape.com www.webmd.com kidshealth.org cme.med.umich.edu www.audiologynet.com