Pharmacology of Local Anesthetics
advertisement
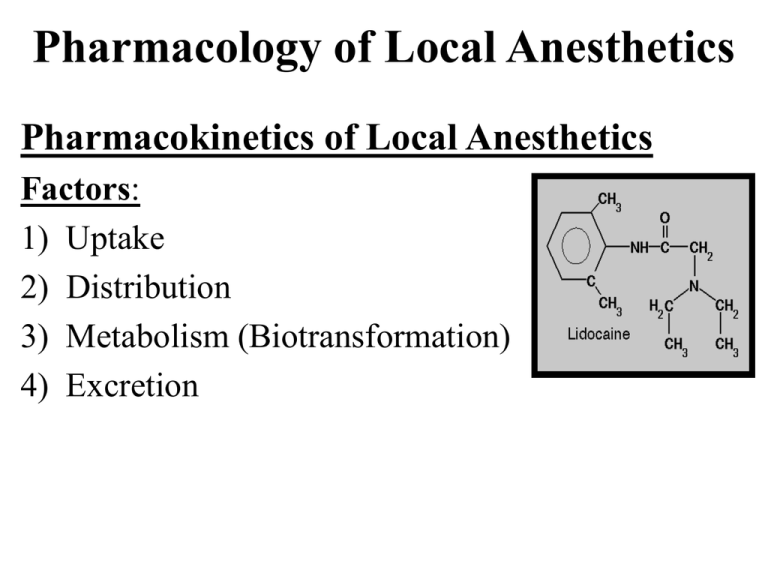
Pharmacology of Local Anesthetics Pharmacokinetics of Local Anesthetics Factors: 1) Uptake 2) Distribution 3) Metabolism (Biotransformation) 4) Excretion Most drugs must enter the circulation to attain therapeutic blood levels before they can exert their clinical action local anesthetics, on the other hand, cease to provide any clinical effect once they leave the site of administration and enter into the blood stream Uptake of Local Anesthetics all local anesthetics possess some degree of vasoactivity; most producing some level of vasodilation ester local anesthetics are potent vasodilating drugs Procaine (Novocaine) possesses tremendous vasodilating abilities which are employed to halt arteriospasm (accidental IA injection) *Cocaine is the only local anesthetic that consistently produces vasoconstriction initial vasodilation intense vasoconstriction vasodilation leads to an increased rate of absorption of the local anesthetic into the blood, thus decreasing the duration and depth of pain control while increasing the anesthetic blood concentration and potential for overdose (toxic reaction) Distribution of Local Anesthetics • once in the blood, local anesthetics are distributed to all tissues • brain, head, liver, lungs, kidneys and spleen have high levels of local anesthetics due to their high level of perfusion • skeletal muscle has the highest level because it has the largest mass of tissue in the body The blood level of local anesthetics is influenced by: 1) Rate at which the drug is absorbed into the cardiovascular system 2) Rate of distribution from the vascular compartment to the tissues 3) Elimination of the drug through metabolic or excretory pathways Elimination Half-Life: the rate at which a local anesthetic is removed from the blood; the time necessary for 50% reduction in the blood level One half life 50% reduction Two half lives 75% reduction Three half lives 87.5% reduction Four half lives 94% reduction Five half lives 97% reduction Six half lives 98.5% reduction All local anesthetics cross the blood brain barrier All local anesthetics cross the placenta and enter the blood stream of the developing fetus PABA Metabolism (ParaAminoBenzoic Acid) Ester Local Anesthetics: plasma pseudocholinesterase hydrolyzed in the plasma by the enzyme pseudocholinesterase the rate of hydrolysis is related to the degree of toxicity Tetracaine is hydrolyzed the slowest which makes it 16 times more toxic than Chloroprocaine which is hydrolyzed the fastest Slower Hydrolyzation = Toxicity Metabolism of Local Anesthetics 2) Amide Local Anesthetics: primary site of metabolism of amide local anesthetics is the liver virtually the entire metabolic process occurs in the liver for Lidocaine, Mepivicaine, Articaine, Bupivacaine and Etidocaine Prilocaine is metabolized in the liver and lung liver function and hepatic perfusion greatly affect the rate of metabolism (biotransformation) of amide local anesthetics significant liver dysfunction (ASA IV/ASA V patients) represents a relative contraindication to the use of amide local anesthetics Articaine has a shorter half-life than other amides because a portion of its metabolism occurs in the blood by plasma cholinesterase Biotransformation of Local Anesthetics 2) Amide Local Anesthetics metabolism byproducts of amide local anesthetics can possess clinical activity if allowed to accumulate in the blood All local anesthetics have the ability to cause sedation Example: large doses of Prilocaine can produce a side effect called Methemoglobinemia; orthotoluidine, a primary metabolite of Prilocaine, induces the formation of methemoglobin Example: large amounts of Lidocaine produce a sedation effect which is due primarily to two metabolites glycine xylidide and monoethylglycinexylidide If the local anesthetic has two “i”s in its name; it’s an amide Lidocaine Prilocaine Bupivacaine Articaine Mepivacaine Esters Amides Plasma Two Types of Contraindications to Drugs: Relative Contraindication: the drug in question may be given to the patient after carefully weighing the risks and benefits Absolute Contraindication: under no circumstance should this drug be administered; toxicity likely Excretion of Local Anesthetics kidneys are the major excretory organs for both local anesthetics esters appear in very small concentrations in the urine; this is because they are almost completely hydrolyzed in plasma Procaine (Novocaine) appears in the urine as 90% PABA and 2% unchanged 10% of Cocaine is found unchanged in the urine patients undergoing dialysis are likely to be unable to excrete the unchanged portion of the esters or amides thus increasing toxicity Systemic Actions of Local Anesthetics the pharmacological action of local anesthetics on the CNS is depression at high levels, local anesthetics will produce tonicclonic convulsions Procaine, Lidocaine, Mepivacaine, Prilocaine and Cocaine generally produce anti-convulsant properties; this occurs at a blood level considerably below that at which the same drugs cause seizures -Procaine, Lidocaine and Mepivacaine have been used therapeutically to terminate or decrease the duration of both grand mal and petit mal seizures; anti-convulsant levels (.5 to 4 micrograms/ml) -The depressant action of local anesthetics raise the seizure threshold by decreasing the excitability of cortical neurons in epileptic patients Preconvulsive Signs and Symptoms numbness of the tongue and circumoral regions anesthetic has been transported to these areas by the cardiovascular system rather than the local delivery of the anesthetic if excitation or sedation occurs in the first 5 to 10 minutes after local anesthetic delivery, it should serve as a warning that convulsive activity could be possible -U.S. Air Force an U.S. Navy pilots are grounded for 24 hours following administration of Lidocaine due to its mild effects of sedation and/or drowsiness -Shivering, slurred speech, muscular twitching, visual/auditory disturbances, dizziness, drowsiness, disorientation and tremor Convulsive Phase o duration of seizures is related to blood level of anesthetic and inversely related to arterial pCO2 levels o at a normal pCO2, a Lidocaine blood level between 7.5 and 10 micrograms/ml usually result in a convulsive episode o when CO2 levels are increased, the blood level of local anesthetic necessary for seizures decreases while the duration of the seizure increases o seizures usually last less than or equal to one minute o cerebral blood flow and cerebral metabolism increase during a seizure o increased blood flow to the brain leads to an increase in the volume of local anesthetic being delivered to the brain causing a longer seizure Convulsive Phase -increased cerebral metabolism leads to acidosis which prolongs the seizure activity even in the presence of declining local anesthetic levels in the blood -seizures gradually subside generalized CNS depression respiratory depression respiratory arrest death How do seizures happen since local anesthetics produce depressant actions on excitable membranes? Answer: local anesthetics produce CNS excitation through a selective blockade of inhibitory pathways in the cerebral cortex; inhibition of inhibition is a pre-synaptic event that follows local anesthetic blockade of impulses traveling along inhibitory pathways; the local anesthetic depresses the action of the inhibitory neurons thus tipping the balance in favor of excessive excitatory input tremor, agitation, seizure and death Convulsive stage CNS depression Cardiovascular Effects of Local Anesthetics local anesthetics have a direct action of the myocardium and peripheral vasculature CVS is more resistant to the effects local anesthetics than the CNS increased local anesthetic blood levels result in decreased myocardial depolarization, however, no change in resting membrane potential and no prolongation of the stages of repolarization local anesthetics decrease myocardial excitation, decrease conduction rate and decrease the force of contraction Lidocaine is used therapeutically for pre-ventricular contractions (PVCs) and ventricular tachycardia local anesthetics cause hypotension from the direct relaxant action on vascular smooth muscle Lung Toxicity local anesthetics have a direct relaxant action on bronchial smooth muscle generally, respiratory function is unaffected by local anesthetics until near overdose levels are achieved Local Tissue Toxicity • skeletal muscle will heal within two weeks of being injected with local anesthetic • longer acting local anesthetics (Bupivacaine) produce more damage to skeletal muscle than do shorter acting agents Malignant Hyperthermia: pharmacogenic disorder in which a genetic variant alters the person’s response to certain drugs. Tachycardia, tachypnea (rapid breathing), unstable blood pressure, cyanosis, fever muscle rigidity and death; 68% mortality rate. Malignant Hyperthermia Association of the U.S. determined that there are no documented cases in Dental or Medical literature supporting the concept of amide local anesthetics triggering malignant hyperthermia References Handbook of Local Anesthesia. Malamed, Stanley. 5th Edition. 2004 “www.mhaus.org”