Brain Protection 12-03-2013 A.N.Hamdy
advertisement
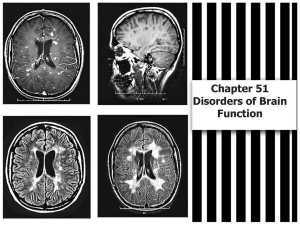
Brain Protection Ahmad N. Hamdy, MD Objectives (IOLs) 1 Cerebral physiology 2 Explain cerebral ischemia Strategies to protect the brain from 3 cerebral ischemia 4 Algorithm for brain protection Cerebral Physiology BRAIN 1350 gm- 2% of total adult body wt Receives 12 to 15 % of cardiac output Global cerebral blood flow 45-55ml/100 gm / min Cortical 75-80ml /100gm/min Subcortical 20ml /100gm/min Cerebral Physiology CMRO2 3 to 3.5 ml/100gm/min Whole brain O2 consumption 50ml/min (20% of total body O2 consumption) Cerebral glucose utilization 5.5 gm/100gm of brain tissue (1ry energy source) ICP ( supine) 5 to 15 mm Hg CPP= MAP- ICP or (CVP), whichever is greater (90-100 mm Hg) Factors Influencing CBF Chemical/Metabolic /Humoral Cerebral metabolic rate Anaesthetics Temperature PaCO2 (20-80 mmHg) PaO2 Vasoactive drugs - Anaesthetics,Vasodilators, Vasopressors Myogenic / Autoregulation Blood viscosity Neurogenic Company Logo Cerebral Ischemia It is the potentially reversible altered state of brain physiology and biochemistry that occurs when substrate delivery is cut off or substantially reduced by vascular stenosis or occlusion Metabolic demands > substrate delivery Pathophysiology Cerebral Ischemia GLOBAL • Cardiac arrest • Resp. Failure • Shock • Hypoglycemia • Asphyxia FOCAL • Head injury • Vascular Stenosis • Occlusion • Spasm Biochemical & Pathophysiological changes Inadequate blood flow ↓↓O2 delivery Ischaemia Excitotoxic cell death Apoptotic cell death Inflammation Strategies for Brain Protection CMRO2 Oxygen Glucose Specific Strategies CBF&CPP Future concepts Oxygen & Glucose In the absence of oxygen, glucose undergoes anaerobic glycolysis resulting in intracellular acidosis Patients with higher blood glucose concentrations have worse outcomes from stroke, TBI, etc. More rapid expansion of ischemic lesion in hyperglycemic, compared with normoglycemic patients For all of this reasons, it is rational to maintain normoglycemia in all patients at risk for ,or recovering from acute brain injury CMRO2 Hypothermia Anesthetics Body Temperature Hyper Ischaemic Injury Hypo Temperature Hypothermia Reduce CMR in a temperature-dependent fashion Mild hypothermia(32-35℃) ; negliable effect on CMR • But, in several studies mild hypothermia produce major protection ; provides scientific basis of using off-bypass hypothermia to provide meaningful neuroprotection Deep hypothermia(18-22℃) ; highly neuroprotective • In normothermic brain ; only a few minutes of complete global ischemia cause neuronal death • In deep hypothermia before circulatory arrest ; brain can tolerate over 40 min and completely or near-completely recover Temperature Hyperthermia In animal studies, spontaneous postischemic hyperthermia is common and intra-ischemic or even delayed post-ischemic hyperthermia dramatically worsen outcome Advocate frequent temperature monitoring in patients with cerebral injuy Aggressive treatment of hyperthermia should be considered Anesthetics Volatile anesthetics Protect against both focal and global ischemia • Transient improvement in global ischemia • Persistent improvement in focal ischemia Suppression of energy requirements • Inhibition of excitatory neurotransmission • Potentiation of inhibitory receptors • Regulation of intracellular calcium response during ischemia Isoflurane, sevoflurane ; Desflurane ; insufficiently studied Company Logo Anesthetics Barbiturates have major actions on CNS: • hypnosis • depression of CMR • anticonvulsant activity. These properties make barbiturates, particularly thiopental, the most commonly used induction agents in neuroanesthesia. Anesthetics Propofol Suppression of CMR Free radical scavenging Anti-inflammatory properties Appears efficacy similar to barbiturates Etomidate Paradoxically exacerbate ischemic injury Cannot use for neuroprotection Lidocaine Suppress CMR Inhibition of apoptosis No long-term outcome studies Ketamine Inhibition of glutamate at NMDA receptor Little or no protection against global insult Substantial protection against focal insult However, no human data CPP More than 65-70mmHg Elevation of MAP Decrease ICP Decrease blood viscosity Specific CCBs as nimodipine (SAH) Na CBs as lamotrigine (SDH) NMDA antagonist Steroids (Brain tumors) Preconditioning Ischaemic Preconditioning Homeothermic mammal Elicits “an evolutionary conserved endogenous response to decreased blood flow and oxygen limitation such as seen during hibernation” Clinical methods of preconditioning Pre - op hyperbaric oxygen Normobaric 100 % oxygen Electroconvulsive shock K+ channel opener→ Diazoxide Erythropoietin (EPO) Erythropoietin Cytokine growth hormone -↓ apoptosis -↑ erythrocyte production ↑↑ haematocrit Deleterious effect on ischaemia Intravenous recombinant erythropoietin Once daily for 3 days 60 -100 fold ↑ of EPO in CNS ↓glial markers of cerebral injury (S 100) ↓ infarct size & improved recovery Astrocytes in ischaemic penumbra produces EPO in mammalian brain Stimulates protein of repair ↓↓neural excitotoxicity Stimulates neurogenesis & angiogenesis ↓neural apoptosis ↓inflammatoin Magnesium Membrane stabilizer Suggested protective mechanism: • • • • • Reduction of presynaptic release of glutamate Blockade of NMDA receptors Smooth muscle relaxation Improved mitochondrial Ca2+ buffering Blockage of Ca2+ entry Protection depends on: • Time of treatment initiation • Type of cerebral ischemia Benefit in neocortical stroke Strategies for Brain Protection O2 • HCT: 30-34 % • PaO2 Levels GL. • 100- 150 mg/dl CMRO2 • Hypothermia • Anesthetics Strategies of Brain Protection (Cont.) CBF • • • • CPP: ≥ 70 mmhg MBP: Elevated Viscosity: Decresed ICP: Decrease Specific • CCBs • Na CBs • NMDA antagonist Future • NO • Cerebral preconditioning • Apoptosis Add your company slogan