CNS 5
advertisement

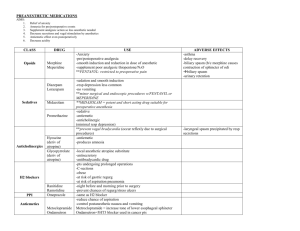
ANESTHETICS SAMUEL AGUAZIM ( MD) 2 3 Patient factors 4 Which influence the selection of the anesthetics are Liver & kidney – target organs for toxic effects by the release of Fluoride, Bromide & other metabolites by halogenated compounds can affect this organ. Respiratory system – if Inhalational anesthetics. CVS – hypotensive effect by most anesthetic agents Nervous system - neurological disorders 5 ANESTHETICS A drug that brings about a reversible loss of consciousness. to induce or maintain general anesthesia to facilitate surgery. Definition 6 Anesthesia: Condition of reversible unconsciousness and absence of response to otherwise painful stimuli. 1. 2. 3. 4. Unconsciousness Analgesia Immobility Amnesia WHAT ARE THE TWO MAJOR CLASSES OF ANESTHETIC AGENTS? * GENERAL * LOCAL General anesthetics are given either as inhaled or intravenous agents. They primarily have CNS effects Local agents are injected at the operative site to block nerve conduction What are the stages of general anesthesia? There are four stages: Stage 1- analgesia- reduced sensation of pain; the patient remains conscious and conversational Stage 11- excitement- delirium and combative behaviour ensue; there is an increase in blood pressure and respiratory rate. Stage 111- surgical anesthesia- the patient is unconscious and regular respiration returns; there is muscle relaxation and decreased vasomotor response to painful stimuli Stage iv- medullary paralysis- respiratory drive decreases and vasomotor output diminishes; death may quickly ensue APPROACHES FOR TESTING DEPTH OF ANAESTHESIA - Blinking of eyelids on striking the eyelashes. - Swallowing - Regularity and depth of respiration. - Increase in respiratory rate and B.P. - Tightness of jaw muscles. Above responses fade on deepening of the anesthesia. 10 What is induction of anesthesia? The time from administration of a general anesthetic to the achievement of surgical anesthesia. Induction is dependent on how fast the anesthetic reaches the CNS RECOVERY IS THE REVERSE OF INDUCTION and it is dependent on how quickly the anesthetic is removed from the CNS Factors that influence the rate of induction for inhaled anesthetics Solubility Pulmonary ventilation Partial pressure of the inhaled agent Alveolar blood flow Arteriovenous concentration gradients INHALED AGENTS HALOTHANE ENFLURANE ISOFLURANE SEVOFLURANE NITROUS OXIDE There potency is defined base on the concept of minimum alveolar concentration ( MAC) What is MAC? Mac is the minimum alveolar concentration of an anesthetic necessary to eliminate movement among 50% of patients challenged by a standardized skin incision The greater the MAC of an agent, the greater the concentration needed to provide anesthesia. Thus an agent with high MAC has low potency ( e.g.. Nitrous oxide) MAC of any inhaled agent can be reduced using it in conjunction with analgesia such as opoid or sedative hypnotics Halothane The first of the halogenated volatile anesthetics to be developed. Clinical use: it is used in the pediatric population because of its pleasant odor and lack of hepatotoxicity. MAC: 0.75% CARDIOVASCULAR EFFECTS OF HALOTHANE It sensitizes the myocardium to the effect of catecholamines ( thus increasing the risk of arrhythmia). Decrease heart rate and cardiac output and leads to lowered BP and peripheral resistance. Toxicity: halothane hepatitis Malignant hyperthermia. What is malignant hyperthermia? A potentially fatal reaction to any of the inhaled anesthetics, which results in hyperthermia, metabolic acidosis, tachycardia and accelerated muscle contraction Treatment : dantrolene and stop the offending agent Enflurane 18 Rapid induction and recovery, less potent than halothane Fewer arrhythmias Greater muscle relaxation Proconvulsant 19 Contraindications/Precautions CI in renal failure. This anesthetic is not used in patients with kidney failure. malignant hyperthermia susceptibility seizure disorder intracranial hypertension Isoflurane 20 Rapid recovery Good muscle relaxation Stable cardiac output Very less effect on heart No rise in ICP. One of the best Inhalational agent.. Isoflurane maintains CO and coronary function better than other agents used in pts with ischemic heart disease. Nitrous oxide 21 1. odorless and non-explosive gas. 2. Anesthetic action. Good analgesia Safe, non irritating Rapid induction due to low solubility. Rapid onset and recovery Negative points: No muscle relaxation Incomplete anesthesia, Must be used in combination .. Toxicity: bone marrow depression with prolonged administration. High concentrations may cause neuropathies INTRAVENOUS AGENTS 22 THIOPENTONE Potent anesthesia High lipid solubility Rapid entry into brain Decreased cerebral blood flow Rapid onset of action Short surgical procedures 23 Thiopentone Negative points: Poor analgesia Little muscle relaxation Laryngospasm Ketamine 24 Good analgesia Dissociative anesthetic. Cardiovascular stimulant Causes disorientation, hallucinations.. Increases cerebral blood flow. 25 Ketamine affects the senses, and produces a dissociative anesthesia (catatonia, amnesia, analgesia) in which the patient may appear awake and reactive, but cannot respond to sensory stimuli. These properties make it especially useful during warfare medical treatment. Used in Trauma and emergency Surgical Procedures also used in high-risk geriatric patients and in shock cases, because it also provides cardiac stimulation. Fentanyl Good analgesia 26 Mostly used with other CNS depressants during anesthesia Because opioids rarely affect the cardiovascular system, they are particularly useful for cardiac surgery Can cause resp. depression and muscle rigidity.. Propofol 27 nonbarbiturate hypnotic agent and the most recently developed intravenous anesthetic. Its rapid induction and short duration of action identical to thiopental. Recovery occurs more quickly and with much less nausea and vomiting 28 29 Rapidly metabolized in the liver and excreted in the urine, so it can be used for long durations of anesthesia, unlike thiopental. Hence, propofol is rapidly replacing thiopental as an intravenous induction agent. Etomidate 30 Ultra short acting non-barbiturate hypnotic No analgesic properties Used for induction followed by other agents Produces postoperative nausea & vomiting Lowers plasma cortisol levels LOCAL ANESTHETICS There are two classes determined by their bonding the lipophilic portion of the molecule with the hydrophilic components- either an ester or amide bond. ANESTHETICS NAME THE ESTER ANESTHETICS NAME THE AMIDE ANESTHETICS COCAINE LIDOCAINE BENZOCAINE MEPIVACAINE PROCAINE BUPIVACAINE TETRACAINE PRILOCAINE Mechanism 33 Block Na channels by binding to specific receptors on inner portion of the channel. First loss of pain, then temp, touch, pressure at the last. 34 Using epinephrine mixed with local anesthetics causes vasoconstriction, which decreases clearance of the agent, increases duration of action, and decreases the total required dosage. USES 35 Short local procedures Spinal anesthesia Minor surgical procedures SE 36 Severe CVS toxicity – Bupivacaine Hypertension & arrhythmias – cocaine CNS excitation Seizures