Acute Kidney Injury - ACH Pediatric Residents
advertisement

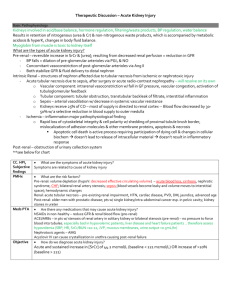
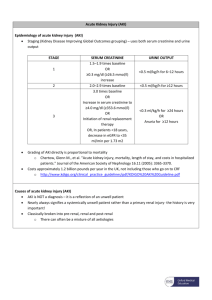
ACUTE RENAL FAILURE Academic Half Day February 9, 2012 Objectives To review: the etiologies of acute kidney injury (AKI) in the pediatric population the work-up/diagnosis of AKI the management of AKI What is AKIs? “abrupt reduction in kidney function as measured by a rapid decline in GFR” Previously known as Acute Renal Failure Now failure represents one end of the spectrum Classification - pRIFLE U/O Risk eCCl dec 25% Injury eCCl dec 50% Failure eCCl dec 75%/ <0.3cc/kg/h x 24h/ < 35ml/min/1.73m2 Anuric x 12h Loss End-stage <0.5cc/kg/h x 8h U/O <0.5cc/kg/h x 16h Persistent failure >4wks Failure > 3 months Leads to: Impaired excretion of nitrogenous waste Impaired water and electrolyte balancing Impaired acid/base regulation Impaired vascular tone regulation Burden of disease Incidence (US): 0.8/100 000; ~1/10 in ICU Increasing Independent risk factor for ICU mortality Increases length of hospital stay May lead to chronic renal failure (40-50% ICU) Etiologies: a general approach Though likely multifactorial, can be divided into: Pre-renal Renal Post-renal Pre-renal causes: Any cause which results from kidney seeing to little blood flow Volume deplete: GI Bleeding Trauma Surgery Vomiting Diarrhea Kidney sees less volume: Sepsis CHF Cirrhosis Vascular - also consider in renal Diuresis Diabetes - DM, DI Drugs RAS Thrombus Takayasu, PAN, KD Drugs NSAIDs ACEi ARBs Renal causes Vascular: Glomerular: Microvasculature: Glomerulonephritis: Acute tubular necrosis •Post-infectious -secondary to nephrotoxic Sickle cell disease HUS Tumour lysis rhabdomyolysis ?Syndromes Hepatorenal Cardiorenal Pulmonary-renal ?Sepsis inflamm, not all volume related •membranoproliferative •SLE •HSP Tubulo/Interstitial: insults or poor perfusion Acute interstitial nephritis -drugs -infxn Cortical dysplasia -hypoxia/ischemia->infarct -toxins/severe HUS Hemolytic Uremic Syndrome History of Ecoli, Shigella, shiga-toxin… Atypical (non-diarrhea, non-shiga-toxin) Hemolytic anemia with fragmented RBCs Thrombocytopenia Renal injury CNS, liver, pancreas can also be affected Post-infectious glomerulonephritis Occurs in ages 5-12, post-GAS. Presentation can be asymptomatic to nephritis complete with gross hematuria, proteinuria, HTN, edema Labs: abnormal urinalysis, low complement Rx: supportive. Prognosis: most make complete recovery. HSP -Causes renal issues d/t IgA deposition. -A/W palpable purpura, arthritis, abdo pain. -Renal more likely to be an issue in older kids -Rx: if crescenteric, GN - steroids. -prognosis: often relapses. Can have late deterioration even if full recovery. 10-30% adults go on to have end-stage disease. Acute Tubular Necrosis Describes an end effect of tubular damage… Secondary to perfusion insults Secondary to toxins Change in blood flow, obstruction and passive filtrate backflow into tubular cells can cause a cycle leading to further death… AIN Drugs (71%) - 1/3 antibiotics Penicillins, cephalosporins, NSAIDs, sulfonamides, cipro, rifampin, PPIs, allopurinol… and more Infection (15%) Strep, Legionella, leptospirosis, CMV, EBV… many Tubulointersitial nephritis and uveitis (5%) Autoimmune: SLE, Sjogren’s Sarcoidosis Idiopathic (8%) Nephrotoxins Vascular effect ACEi, cyclosporine, tacrolimus Tubular effect AIN Proximal: aminoglycosides, amphotericin B, cisplatin, immunoglobulins, contrast Distal: NSAIDs, ACEi, lithium, cyclophosphamide Obstruction: sulfa, acylovir, methotrexate Post-renal causes Two kidneys - distal or bilateral proximal obstruction Single kidney - obstruction anywhere Posterior urethral valves Ureteropelvic junction obstruction Ureterovesicular junction obstruction Ureterocele Stones Tumour Hemorrhagic cystitis Neurogenic bladder On history… ? pre-renal: Vomiting, diarrhea, bleeding, sepsis, dec PO Drug use - inc NSAIDs ? renal: Bloody diarrhea? (HUS) Recent illness? (PSGN) Crush injury? Drug use: aminoglycosides, antifungals, chemo Associated lung/heart/liver symptoms? (dual organ) ? post-renal: On physical… Pre-renal: Dehydration Signs of heart failure/cirrhosis/sepsis Renal: Edema (nephrotic syndrome) Purpura (HSP Post-renal: palpable bladder? What to order? BUN, Cr, lytes, fractional excretion of sodium Urinalysis On labs… Everyone gets a urinalysis… NORMAL: -pre-renal (may be concentrated) -post-renal -ATN ABNORMAL: -brown granular/epithelial casts = ATN -red cell casts = glomerulonephritis -proteinuria = glomerular -pyuria, white cell casts = UTI or glomerulonephritis (postinfxn) -hematuria = AIN, vasculitis, infarction, obstruction And even more information from urine… Urine osmolality: Typically low in ATN (<350 mosmol/kg) Typically high in pre-renal disease (>500) Urine volume: Often low, especially given criteria for AKI. However, some ATN is non-oliguric Urine eosinophils Urine sodium… Sodium excretion Why? Helps distinguish pre-renal vs ATN… >30-40 mEq/L = ATN <10 mEq/L = effective volume depletion (20-30 in infants) BUT what if there is a large urine output? Fractional Excretion of Sodium FENa compensates for the urine output… UNa x PCr PNa x UCr …can also be thought of as UNa/PNa UCr/PCr <1% --> pre-renal disease 1-2% --> ?? >2% --> ATN Bloodwork… CBC: look for MAHA, thrombocytopenia Extended lytes. Renal injury can result in: Hyperkalemia Hyperphosphatemia Hypocalcemia Metabolic acidosis Other options, depending on history: ANCA, ANA, ASOT, complement, drug levels… And of course, creatinine Creatinine is usually elevated Normal Cr varies by age Age Normal range (umol/L) Newborn 27-88 Infant 18-35 Child 27-62 Adolescent 44-88 Note Cr can NOT be used to estimate GFR in acute kidney injury… This is why the search is on for a “troponin of the kidneys” Troponin of the kidneys? Unfortunately, not yet… Some ideas: Urinary neutrophil gelatinase-associated lipocalin (NGAL) Increased 50-fold, and 24h before serum Cr Has been shown to predict AKI severity in SLE, HUS, renal transplant patients Kidney injury molecule - 1 (KIM-1) IL-18 Imaging Ultrasound - in all children if etiology unclear # of kidneys Size of kidneys Obvious parenchymal damage Obstruction Thrombus/vessel occlusion Renal biopsy Only when diagnosis remains unknown, or there is a failure to respond to treatment Approach summary: pRIFLE met -estimated CrCl -oliguria NORMAL urinalysis ABNORMAL urinalysis Ultrasound PRE-RENAL Low ECF volume -GI loss -diuresis -hemorrhage RENAL POST-RENAL Low vol to kidney -bilateral ureteric obstruction -heart failure -single kidney + ureter obs -m eds (NSAIDs, ACEi, ARB) -bladder/urethra obs -vascular disease Vascular disorders Artery -RAS -Takayasu, PAN, KD -can think of drugs here too Veins -thrombosis Parenchymal disorders Glomerular disorders Tubular disorders AIN -drugs -infection -autoimmune ATN -ischemia -contrast plugged -crystals -globins -drugs Treatment Principles: 1. FEN 2. Avoid complications 3. Treat underlying cause Generally pediatric nephrology will be involved. FEN - fluids Child can be hypo-, eu- or hypervolemic. FLUID STATUS Hypovolemia Goal: maintain renal perfusion Euvolemia Hypervolemia Type Title Here Crystalloids (NS) -bolus, rpt -no change? Consider invasive monitors Monitor ins/outs -daily weights -ins=outs + insensibles Fluid removal/restriction -furosemide (2-5mg/kg) -no change? Consider RRT HTN can occur and is usually secondary to volume overload. Treatment based on diuretic response, severity. FEN - electrolytes Hyperkalemia - if severe (>7) - C BIG K Die… Don’t give K (IVs, low K diet) stabilize the cardiac membrane - IV calcium gluconate Move K ECF -> ICF by: Insulin (with glucose) Sodium bicarb Beta agonists Remove K from the body - kayexalate Can try diuretics - unlikely to do enough RRT if the above doesn’t work FEN - electrolytes Acidosis Respiratory compensation can be enough Sodium bicarb ONLY if life-threatening and/or contributing to hyperkalemia Def not if pH >7.2 or bicarb >14mEq/L Can decrease Ca further -> seizures Can increase intravascular volume If refractory volume overload, hypernatremia -> RRT FEN - electrolytes Hyperphosphatemia: Low phosphate diet Binders Hypocalcemia: Calcium gluconate Can pre-empt if sodium bicarb being given FEN - Nutrition AKI is a catabolic state Ensure adequate calories - 120kcal/kg/d in infants - usual maintenance for children PO -> enteral -> TPN If fluid balance off with adequate nutrition: RRT Avoid complications Including making things worse…so no: Aminoglycosides NSAIDs Antifungals Immunosuppressive drugs Contrast media Renal Replacement Therapy (RRT) Indications: 1. Uremia s/s - pericarditis, neuropathy, decline 2. Azotemia - BUN >36 3. Refractory fluid overload - HTN, pulm edema, CHF 4. Refractory hyperK, hypo/hyperNa, acidosis 5. Nutritional support with fluid balance issues RRT Options: Continuous renal replacement therapy Peritoneal dialysis Hemodialysis Prognosis Mortality: 60% (critically ill) 20-25% go on to have some degree of chronic renal issues Take home points Etiology: Best divided into pre-, renal and post-renal Work-up: Urinalysis, ultrasound, bloodwork… Treatment: Fluids - close balance Electrolytes - esp K, PO4, Ca Acidosis Nutrition Dialysis - talk later today References Akcan-Arikan A, Zappitelli M, Loftis L, Washburn K, Jerrerson L, and Goldstein S. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney International; 2007: 71: 1028-35. Basu R, Devarajan P, Wong H, and Wheeler S. An update and review of acute kidney injury in pediatrics. Pediatric Critical Care Medicine; 2011: 12(3): 339-47. Imam A. Clinical presentation, evaluation, and diagnosis of acute kidney injury (acute renal failure) in children. Uptodate. Accessed Feb 8, 2012 at http://www.uptodate.com.ezproxy.lib.ucalgary.ca/contents/clinical-presentation-evaluation-anddiagnosis-of-acute-kidney-injury-acute-renal-failure-inchildren?source=search_result&search=acute+kidney+injury&selectedTitle=2~150 Imam A. Prevention and management of acute kidney injury (acute renal failure) in children. Uptodate. Accessed Feb 8, 2012 at http://www.uptodate.com.ezproxy.lib.ucalgary.ca/contents/prevention-and-management-of-acutekidney-injury-acute-renal-failure-inchildren?source=search_result&search=acute+kidney+injury&selectedTitle=1~150 Kliegman R, Stanton B, Geme J, Schor N, and Behrman R. Nelson Textbook of Pediatrics 19th e. Elsevier; 2011: 1814-22.