Therapeutic Discussion – Acute Kidney Injury
advertisement
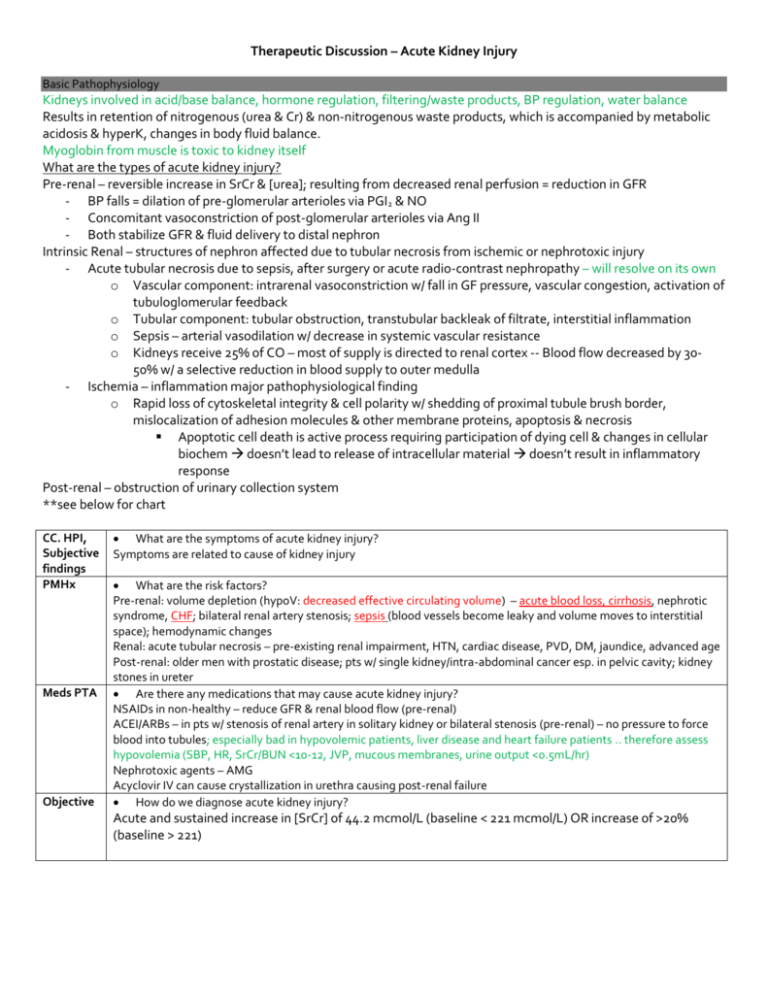
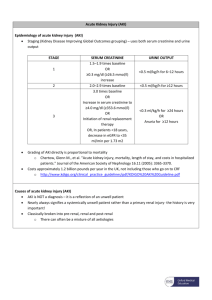
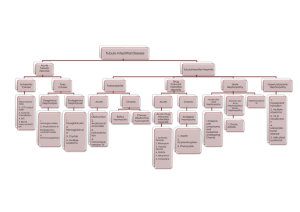
Therapeutic Discussion – Acute Kidney Injury Basic Pathophysiology Kidneys involved in acid/base balance, hormone regulation, filtering/waste products, BP regulation, water balance Results in retention of nitrogenous (urea & Cr) & non-nitrogenous waste products, which is accompanied by metabolic acidosis & hyperK, changes in body fluid balance. Myoglobin from muscle is toxic to kidney itself What are the types of acute kidney injury? Pre-renal – reversible increase in SrCr & [urea]; resulting from decreased renal perfusion = reduction in GFR - BP falls = dilation of pre-glomerular arterioles via PGI2 & NO - Concomitant vasoconstriction of post-glomerular arterioles via Ang II - Both stabilize GFR & fluid delivery to distal nephron Intrinsic Renal – structures of nephron affected due to tubular necrosis from ischemic or nephrotoxic injury - Acute tubular necrosis due to sepsis, after surgery or acute radio-contrast nephropathy – will resolve on its own o Vascular component: intrarenal vasoconstriction w/ fall in GF pressure, vascular congestion, activation of tubuloglomerular feedback o Tubular component: tubular obstruction, transtubular backleak of filtrate, interstitial inflammation o Sepsis – arterial vasodilation w/ decrease in systemic vascular resistance o Kidneys receive 25% of CO – most of supply is directed to renal cortex -- Blood flow decreased by 3050% w/ a selective reduction in blood supply to outer medulla - Ischemia – inflammation major pathophysiological finding o Rapid loss of cytoskeletal integrity & cell polarity w/ shedding of proximal tubule brush border, mislocalization of adhesion molecules & other membrane proteins, apoptosis & necrosis Apoptotic cell death is active process requiring participation of dying cell & changes in cellular biochem doesn’t lead to release of intracellular material doesn’t result in inflammatory response Post-renal – obstruction of urinary collection system **see below for chart CC. HPI, Subjective findings PMHx Meds PTA Objective What are the symptoms of acute kidney injury? Symptoms are related to cause of kidney injury What are the risk factors? Pre-renal: volume depletion (hypoV: decreased effective circulating volume) – acute blood loss, cirrhosis, nephrotic syndrome, CHF; bilateral renal artery stenosis; sepsis (blood vessels become leaky and volume moves to interstitial space); hemodynamic changes Renal: acute tubular necrosis – pre-existing renal impairment, HTN, cardiac disease, PVD, DM, jaundice, advanced age Post-renal: older men with prostatic disease; pts w/ single kidney/intra-abdominal cancer esp. in pelvic cavity; kidney stones in ureter Are there any medications that may cause acute kidney injury? NSAIDs in non-healthy – reduce GFR & renal blood flow (pre-renal) ACEI/ARBs – in pts w/ stenosis of renal artery in solitary kidney or bilateral stenosis (pre-renal) – no pressure to force blood into tubules; especially bad in hypovolemic patients, liver disease and heart failure patients .. therefore assess hypovolemia (SBP, HR, SrCr/BUN <10-12, JVP, mucous membranes, urine output <0.5mL/hr) Nephrotoxic agents – AMG Acyclovir IV can cause crystallization in urethra causing post-renal failure How do we diagnose acute kidney injury? Acute and sustained increase in [SrCr] of 44.2 mcmol/L (baseline < 221 mcmol/L) OR increase of >20% (baseline > 221) Vitals Physical Exam Investigations Vitals, CNS, HEENT: if hypovolemic GU: acute anuria/severe oliguria (pre-renal: oliguria <400 mL/day; post-renal/renal: any); renal U/S will show hydronephrosis in post-renal failure Lab SrCr – depends on urinary Cl of Cr & on rate of production & Vd – doesn’t accurately reflect GFR in non-SS condition of acute renal failure; best marker is urine output! Tubular necrosis w/ intact tubular function: fractional excretion of filtered Na <1% - If not: fractional excretion > 2-3% Acute allergic interstitial nephritis: hypersensitivity rxn (fever, rash, arthralgias); urine contains WBC, RBC, white cell casts; fractional excretion of Na >1%; eosinophilia (except NSAIDs); mostly caused by B-lactam abx and Septra Pre-renal: fractional excretion of uric acid & lithium <7% (more specific than Na for prerenal); urine volume & Na excretion are low Goals of therapy D/C the offending agent Prevent pre-renal failure to progress to ischemic acute tubular necrosis 1. Look at post-renal causes first 2. Then look at pre-renal causes (i.e. volume status) 3. Then lastly look at intrinsic causes Treatment alternatives and duration Prevention & treatment of associated complications - HyperK: IV Ca; NaHCO3, glucose & insulin (drives K into cells) don’t remove K from body o Additional tx w/ Na-K exchange resin (ie. Kayexalate) or dialysis - Oliguric – daily fluid intake limited to 400 mL + prev. urinary output - Dietary Na restricted to 2g/day - Acidosis – NaHCO3 if conc < 15-19 mmol/L - HyperP – CaCO3 or other phosphate binders o Severe – treat w/ dialysis Dialysis: (cont. > intermittent HD) Non-oliguric: >450 mL/day Oliguria: urine output <200 mL/12 hr (50-450 mL/day) Anuria: urine output <50 mL/12 hr HyperK: K >6.5 mmol/L Severe acidemia: pH <7 Azotemia: urea conc >30 mmol/L Uremic encephalopathy, neuropathy/myopathy, pericarditis Plasma Na: >155 mmol/L or <120 mmol/L Hyperthermia Drug overdose w/ dialyzable toxin Post-renal – BPH & crystallization put catheter in Pre-renal – STOP DRUG; replace intravascular space with NS (250mL will go into space), but caveat is that in cirrhosis/HF you are also increasing their interstitial volume; should see a decrease in SrCr within 1 day Post-renal – treat the underlying cause; ensure volume is restored; allow kidneys to recover on their own Acute allergic interstitial nephritis – stop offending agent, and then may try steroid therapy x 4-6 weeks, then try cyclophosphamide Mannitol – prevented acute renal fx only in rhabdomyolysis & kidney-transplant surgey Low-dose dopamine – renal vasodilator; doesn’t reduce mortality/promote recovery of renal fx; option in septic shock Acetylcysteine PO – w/ hydration lowers risk of contrast nephropathy in chronic renal insufficiency; also affects tubular handling of Cr (so decrease in SrCr conc. doesn’t lead to protective effect on GFR) CCB – no evidence Monitoring Parameters: Efficacy and toxicity Efficacy: SrCr, BUN, lytes, urine output Acute glomerulonephritis – protein leakage