audit cycle to improve the clinical assessment of patients with acute
advertisement
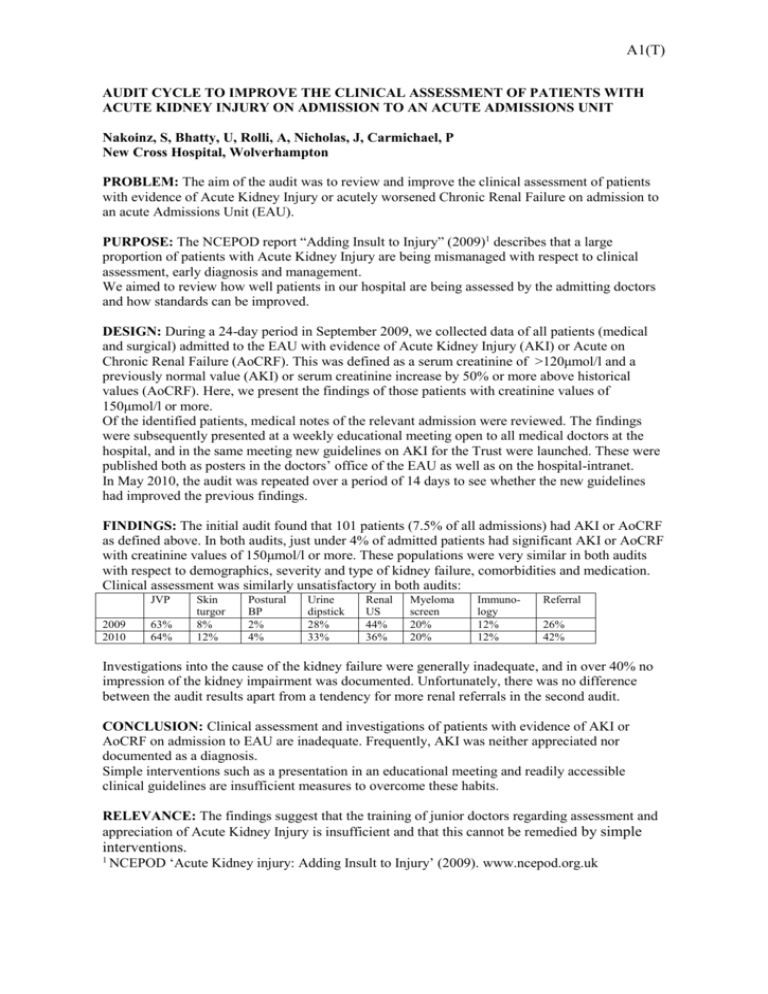
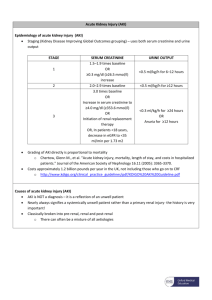
A1(T) AUDIT CYCLE TO IMPROVE THE CLINICAL ASSESSMENT OF PATIENTS WITH ACUTE KIDNEY INJURY ON ADMISSION TO AN ACUTE ADMISSIONS UNIT Nakoinz, S, Bhatty, U, Rolli, A, Nicholas, J, Carmichael, P New Cross Hospital, Wolverhampton PROBLEM: The aim of the audit was to review and improve the clinical assessment of patients with evidence of Acute Kidney Injury or acutely worsened Chronic Renal Failure on admission to an acute Admissions Unit (EAU). PURPOSE: The NCEPOD report “Adding Insult to Injury” (2009)1 describes that a large proportion of patients with Acute Kidney Injury are being mismanaged with respect to clinical assessment, early diagnosis and management. We aimed to review how well patients in our hospital are being assessed by the admitting doctors and how standards can be improved. DESIGN: During a 24-day period in September 2009, we collected data of all patients (medical and surgical) admitted to the EAU with evidence of Acute Kidney Injury (AKI) or Acute on Chronic Renal Failure (AoCRF). This was defined as a serum creatinine of >120μmol/l and a previously normal value (AKI) or serum creatinine increase by 50% or more above historical values (AoCRF). Here, we present the findings of those patients with creatinine values of 150μmol/l or more. Of the identified patients, medical notes of the relevant admission were reviewed. The findings were subsequently presented at a weekly educational meeting open to all medical doctors at the hospital, and in the same meeting new guidelines on AKI for the Trust were launched. These were published both as posters in the doctors’ office of the EAU as well as on the hospital-intranet. In May 2010, the audit was repeated over a period of 14 days to see whether the new guidelines had improved the previous findings. FINDINGS: The initial audit found that 101 patients (7.5% of all admissions) had AKI or AoCRF as defined above. In both audits, just under 4% of admitted patients had significant AKI or AoCRF with creatinine values of 150μmol/l or more. These populations were very similar in both audits with respect to demographics, severity and type of kidney failure, comorbidities and medication. Clinical assessment was similarly unsatisfactory in both audits: JVP 2009 2010 63% 64% Skin turgor 8% 12% Postural BP 2% 4% Urine dipstick 28% 33% Renal US 44% 36% Myeloma screen 20% 20% Immunology 12% 12% Referral 26% 42% Investigations into the cause of the kidney failure were generally inadequate, and in over 40% no impression of the kidney impairment was documented. Unfortunately, there was no difference between the audit results apart from a tendency for more renal referrals in the second audit. CONCLUSION: Clinical assessment and investigations of patients with evidence of AKI or AoCRF on admission to EAU are inadequate. Frequently, AKI was neither appreciated nor documented as a diagnosis. Simple interventions such as a presentation in an educational meeting and readily accessible clinical guidelines are insufficient measures to overcome these habits. RELEVANCE: The findings suggest that the training of junior doctors regarding assessment and appreciation of Acute Kidney Injury is insufficient and that this cannot be remedied by simple interventions. 1 NCEPOD ‘Acute Kidney injury: Adding Insult to Injury’ (2009). www.ncepod.org.uk