Acute kidney injury
advertisement

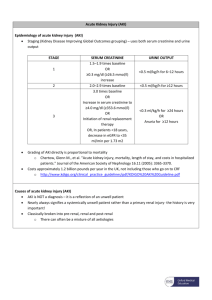
Do we know what we mean? There are more than 35 definitions of AKI (formerly acute renal failure) in literature! Mehta R, Chertow G: Acute renal failure definitions and classification: Time for change? Journal of American Society of Nephrology 2003; 14:2178-2187. RIFLE classification AKIN classification Bellomo R, Ronco C, Kellum J, et al.: Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Initiative (ADQI) Group. Critical Care 2004; 8:R204-R212. Modification of the RIFLE classification by Acute Kidney Injury Network (AKIN). Recognizes that small changes in serum creatinine (>0.3 mg/dl) adversely impact clinical outcome. Uses serum creatinine, urinary output and time. Coca S, Peixoto A, Garg A, et al.: The prognostic importance of a small acute decrement in kidney function in hospitalized patients: a systematic review and meta-analysis. American Journal of Kidney Diseases 2007; 50:712720. AKIN Serum Creatinine stage Criteria Urinary Output Time Criteria 1 Cr ≥ 0.3 mg/dL or ≥ 150-200% from baseline < 0.5 mL/kg/hr > 6 hrs 2 Cr to > 200-300% from baseline < 0.5 mL/kg/hr > 12 hrs 3 Cr to > 300% from baseline or Cr ≥ 4mg/dL with an acute rise of at least 0.5 mg/dL < 0.5 mL/kg/hr or anuria X 24 hrs X 12 hrs *Patients needing RRT are classified stage 3 despite the stage they were before starting RRT Mehta R, Kellum J, Shah S, et al.: Acute kidney Injury Network: Report of an Initiative to improve outcomes in Acute Kidney Injury. Critical Care 2007; 11: R31. AKI is an abrupt (within 48 hrs) reduction in kidney function currently defined as an absolute increase in serum creatinine of ≥ 0.3 mg/dL (≥ 26.4 μmol/L), a percentage increase in serum creatinine of ≥ 50%, or a reduction in urine output (documented oliguria of < 0.5 mL/kg/hr for > 6hrs. Mehta R, Kellum J, Shah S, et al.: Acute kidney Injury Network: Report of an Initiative to improve outcomes in Acute Kidney Injury. Critical Care 2007; 11: R31. AKI occurs in ≈ 7% of hospitalized patients. 36 – 67% of critically ill patients (depending on the definition). 5-6% of ICU patients with AKI require RRT. Nash K, Hafeez A, Hou S: Hospital-acquired renal insufficiency. American Journal of Kidney Diseases 2002; 39:930-936. Hoste E, Clermont G, Kersten A, et al.: RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: A cohort analysis. Critical Care 2006; 10:R73. Osterman M, Chang R: Acute Kidney Injury in the Intensive Care Unit according to RIFLE. Critical Care Medicine 2007; 35:1837-1843. Mortality increases proportionately with increasing severity of AKI (using RIFLE). AKI requiring RRT is an independent risk factor for in-hospital mortality. Mortality in pts with AKI requiring RRT 5070%. Even small changes in serum creatinine are associated with increased mortality. Hoste E, Clermont G, Kersten A, et al.: RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: A cohort analysis. Critical Care 2006; 10:R73. Chertow G, Levy E, Hammermeister K, et al.: Independent association between acute renal failure and mortality following cardiac surgery. American Journal of Medicine 1998; 104:343-348. Uchino S, Kellum J, Bellomo R, et al.: Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA 2005; 294:813818. Coca S, Peixoto A, Garg A, et al.: The prognostic importance of a small acute decrement in kidney function in hospitalized patients: a systematic review and meta-analysis. American Journal of Kidney Diseases 2007; 50:712-720. Serum Creatinine Urine Output Time Dennen P, Douglas I, Anderson R,: Acute Kidney Injury in the Intensive Care Unit: An update and primer for the Intensivist. Critical Care Medicine 2010; 38:261-275. Sepsis Major surgery Low cardiac output Hypovolemia Medications (20%) Uchino S, Kellum J, Bellomo R, et al.: Acute renal failure in critically ill patients: A multinational, multicenter study. JAMA 2005; 294:813-818. Hepatorenal syndrome Trauma Cardiopulmonary bypass Abdominal compartment syndrome Rhabdomyolysis Obstruction Dennen P, Douglas I, Anderson R,: Acute Kidney Injury in the Intensive Care Unit: An update and primer for the Intensivist. Critical Care Medicine 2010; 38:261-275. NSAIDs Aminoglycosides Amphotericin Penicillins Acyclovir Cytotoxics Radiocontrast dye Dennen P, Douglas I, Anderson R,: Acute Kidney Injury in the Intensive Care Unit: An update and primer for the Intensivist. Critical Care Medicine 2010; 38:261-275. Recognition of underlying risk factors ◦ ◦ ◦ ◦ ◦ Diabetes CKD Age HTN Cardiac/liver dysfunction Maintenance of renal perfusion Avoidance of hyperglycemia Avoidance of nephrotoxins Dennen P, Douglas I, Anderson R,: Acute Kidney Injury in the Intensive Care Unit: An update and primer for the Intensivist. Critical Care Medicine 2010; 38:261-275. Avoid use of intravenous contrast in high risk patients if at all possible. Use pre-procedure volume expansion using isotonic saline (?bicarbonate). NAC Avoid concomitant use of nephrotoxic medications if possible. Use low volume low- or iso-osmolar contrast Dennen P, Douglas I, Anderson R,: Acute Kidney Injury in the Intensive Care Unit: An update and primer for the Intensivist. Critical Care Medicine 2010; 38:261-275. Intravenous albumin significantly reduces the incidence of AKI and mortality in patients with cirrhosis and SBP. Albumin decreases the incidence of AKI after large volume paracentesis. Albumin and terlipressin decrease mortality in HRS. Sort P, Navasa M, Arroyo V, et al.: Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. New England Journal of Medicine 1999; 341:403-409. Gines P, Tito L, Arroyo V, et al.: Randomised comparative study of therapeutic paracentesis with and without intravenous albumin in cirrhosis. Gastroenterology 1988; 94:1493-1502. Gluud L, Kjaer M, Christensen E: Terlipressin for hepatorenal syndrome. Cochrane Database Systematic Reviews 2006; CD005162. Maintain renal perfusion Correct metabolic derangements Provide adequate nutrition ? Role of diuretics Human kidney has a compromised ability to autoregulate in AKI. Maintaining haemodynamic stability and avoiding volume depletion are a priority in AKI. Kelleher S, Robinette J, Conger J: Sympathetic nervous system in the loss of autoregulation in acute renal failure. American Journal of Physiology 1984; 246: F379-386. Current studies do not include patients with established AKI. The individual BP target depends on age, comorbidities (HTN) and the current acute illness. A generally accepted target remains MAP ≥ 65. Bourgoin A, Leone M, Delmas A, et al.: Increasing mean arterial pressure in patients with septic shock: Effects on oxygen variables and renal function. Critical Care Medicine 2005; 33:780-786. SAFE study – no statistical difference between volume resuscitation with saline or albumin in survival rates or need for RRT. Post – hoc analysis – albumin was associated with increased mortality in traumatic brain injury subgroup and improved survival in septic shock patients. Finfer S, Bellomo R, Boyce N, et al.: A comparison of albumin and saline for fluid resuscitation in the intensive care unit. New England Journal of Medicine 2004; 350: 2247-2256. Fluid conservative therapy decreased ventilator days and didn’t increase the need for RRT in ARDS patients. Association between positive fluid balance and increased mortality in AKI patients. Wiedeman H, Wheeler A, Bernard G, et al.: Comparison of two fluid management strategies in acute lung injury. New England Journal of Medicine 2006; 354:2564-2575. Payen D, de Pont A, Sakr Y, et al.; A positive fluid balance is associated with worse outcome in patients with acute renal failure. Critical Care 2008; 12: R74. There is no evidence that from a renal protection standpoint, there is a vasopressor agent of choice to improve kidney outcome. Dennen P, Douglas I, Anderson R,: Acute Kidney Injury in the Intensive Care Unit: An update and primer for the Intensivist. Critical Care Medicine 2010; 38:261-275. “Renal” dose dopamine doesn’t reduce the incidence of AKI, the need for RRT or improve outcomes in AKI. It may worsen renal perfusion in critically ill adults with AKI. Side effects of dopamine include increased myocardial oxygen demand, increased incidence of atrial fibrillation and negative immuno-modulating effects. Lauschke A, Teichgraber U, Frei U, et al.: “Low-dose” dopamine worsens renal perfusion in patients with acute renal failure. Kidney 2006; 69:1669-1674. Argalious M, Motta P, Khandwala F, et al.: “Renal dose” dopamine is associated with the risk of new onset atrial fibrillation after cardiac surgery. Critical Care Medicine 2005; 33:1327-1332.