Stress Dose Steroids - Clinical Departments
advertisement
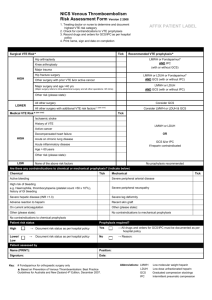
Perioperative Medicine Beyond Cardiac Clearance Pamela Pride MD July 31, 2012 MUSC Objectives Define the management of anticoagulation List the VTE risk factors List the modes of prophylaxis Differentiate stress dose steroids Identify causes and management of postoperative fever Key Messages Patients on chronic anticoagulation with high risk of thrombosis should be bridged preoperatively with short acting anticoagulation (i.e. heparin gtt or enoxaparin) Recommending LMWH for post op DVT prophylaxis is rarely incorrect. Recommendations regarding stress dose steroids for patients on chronic glucocorticoids are available, although data supporting their routine use is lacking. Fevers in the first 48 hours post op are common and routine work up with chest xray, blood and urine cultures is not indicated in an otherwise asymptomatic patient. Perioperative Medicine Beyond Cardiac Clearance Management of anticoagulation VTE prophylaxis Stress dose steroids Postoperative fever Antiplatelet Therapy and Surgery Anticoagulation and Surgery To bridge or not bridge Don’t Bridge Bridge Dual prosthetic or old valve VTE w/in 3 months Pregnancy and PV PV with embolism in past 6 months Afib with chad score ≥ 5 Bileaflet valve with additional risk factors Bileaflet AV VTE >12 months ago Afib with chad score ≤ 2 and no hx of cva/tia Venous Thromboembolism Prophylaxis VTE Risk Factors Surgery Trauma Immobility Malignancy Hx of VTE Advanced age Pregnancy/HRT Organ failure IBD Nephrotic syndrome Myeolproliferative d/o PNH Obesity Tobacco abuse Varicose veins CV catheters Thrombophilia Modes Of Prophylaxis LDUH LMWH ASA Coumadin GCS Foot pumpers Fondaparinux Early mobilization IPC IVC filter VTE Prophylaxis Made Easy “KISS” Recommend LMWH unless risk of bleeding is high, then use mechanical prophylaxis However……………. VTE Prophylaxis Special Circumstances Warfarin vs. LMWH vs. fondaparinux How long to treat? Hips Knees Bariatric surgery Renal insufficiency HIT Adrenal Physiology Baseline daily cortisol secretion 8-10mg Surgical stress increases baseline secretion Exogenous steroids inhibit CRH and ACTH secretion Adrenal atrophy may result and blunt normal response Who is at risk for HPA suppression? Assume suppression Greater than 20mg/d prednisone for more than 3 weeks Clinically Cushingoid Assume No Suppression Any dose for less than 3 weeks Less than 5mg/d prednisone for any duration Alternate day regimen Stress Dose Steroids Minor surgical stress Moderate surgical stress Take usual morning dose Take usual morning dose plus 50mg IV HCT prior to surgery and 25mg IV q8hours for 3 doses Major surgical stress Take usual am dose plus 100mg IV HCT prior to surgery and 50mg IV q8 for 3 doses, then taper by 50% each day What does the data show? Data limited by few RCTs and low sample sizes 1-2% incidence of adrenal insufficiency when steroids completely withheld No difference between stress dose and maintenance dose Patients with adrenal crisis respond to “rescue” stress dose steroids Surgical Patients on Chronic Steroids-Summary Post op adrenal insufficiency is a rare but serious complication With holding steroids completely leads to higher rates of crisis Data suggests that maintenance dosing with close post-op monitoring is advisable If decision is made to give stress dose steroids, follow previous listed recs Postoperative Fever Common, related to cytokines History and physical exam only recommended for first 48 hours postop References Vinik R, et al. Periprocedural antithrombotic management:A review of the literature and practical approach for the hospitalist physician. J Hosp Med 4(9) 551-9 November 2009 Guyatt, G, et al. Antithrombotic Therapy and Prevention of Thombosis 9th Ed: ACCP Guidelines. Chest November 2012 Issue 2 Supplement Badillo A, Sarani B, and S Evans. Optimizing Use of Blood Cultures in the Febrile Postoperative patient. J Am Coll Surg 194(4):477 2002 Axelrod L. Perioperative Management of Patients treated with glucocorticoids. Endocrinol Metab Clin North Am. June 32(2)367:-83 2003.