Presentation - Neuro
advertisement

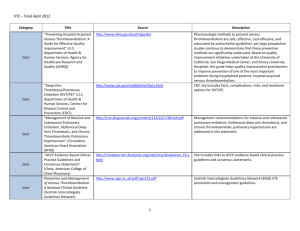
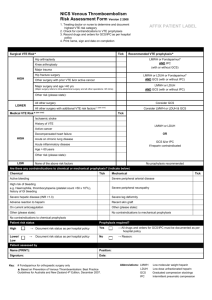
Neuro-Onc SIG Meeting Venous Thromboembolic Events Care Strategies for the Neuro-Oncology Patient Neuro-Onc SIG Meeting I. II. Agenda Introduction & Welcome CEU Presentation: Venous Thromboembolic Events Care Strategies for the Neuro-Oncology Patient III. SIG Meeting Venous Thromboembolic Events Care Strategies for the Neuro-Oncology Patient A Neu-Onc SIG CEU presentation Mary Elizabeth Davis, RN, MSN, AOCNS Clinical Nurse Specialist MSKCC davism@mskcc.org Venous Thromboembolic Events VTE stats: • Includes PE and DVT • 3rd most common cardiovascular illness • Approx 1 million/year in US • 2/3 result from hospitalization: approx 300K die • PE - most common preventable cause of hospital related death • 2nd leading cause of death in patients with active cancer (possibly 1st) Stats Specific for Glioma : • Semrad, et.al. (2007) -9489 malignant glioma pts - 7.5% had VTE within first 6mos dx (55% within 2 months post-op) - Associated with poorer prognosis -+ VTE = 30% ↑ risk death within 2yrs • Risk-3-60% first 6 wks after sx then 24% over life (Batchelor & Byrne, 2006, Jenkins, et. al, 2010, Marras, Geerts & Perry, 2000) Specific for Glioma Proposed pathophysiology: • Higher plasma levels of thrombosis associated biomarkers (D-dimer, lipoprotein A, VEGF, tissue plasminogen factor(tPA), PAI-1) • Pathologic specimens: intra-lumen thrombosis common (distorted vasculature, increased interstitial pressure) • Surgical resection make cause release of procoagulant microparticles into circulation & post-op immobility/ paresis may further contribute Jenkins, et al., 2010, Sartori, et al,2011) Consequences of VTE • Inpatient hospitalization • Interruption of cancer treatment • Need for pharmacologic management- chronic anticoagulation - financial burden - ↑ risk of bleeding • ↑ risk of recurrent DVT (PTS) • ↓ QOL • ↓ survival - likelihood of death 2-6x > for patients with cancer who have VTE Risk of VTE • Active cancer Dx • 4-7x > risk VTE than no Ca (Aikens, Rivey & Hansen, 2013) • Hi risk Cas: Pancreatic, gastric, brain, myeloproliferative • √ Malignant Gliomas • Histology: Adeno > SCC • N/A, but …GBM 5x> other brain histology (such as AA, AO) (Brandes et al 1997) • Metastatic Dx 2x > local disease • N/A PBTs- rarely metastasize outside CNS • Previous h/o DVT • ? Patient specific Risk of VTE • Cancer treatment • Surgical procedures • Chemotherapy Risk AnalysisChemotherapy Predictive model (Khorana et.al 2008) • Glucocorticoids (Johannesdottir, et al, 2013) • √ brain tumors • ↑ risk surgery> 4 hours • Subtotal resection > total • Larger tumor size (5cm) • √ high grade Gliomas • esp bevacizumab NCCN 5 clinical lab parameters - site of cancer - pre chemo plt ct > 350x109 /L - hgb < 10g/dL (or use ESA) - leukocyte ct > 11 x 109/L - BMI > 35kg/m2 • √ brain tumors Risk of VTE • Immobility • √ Gliomas –especially leg paresis; DVT more likely in paretic limb (Brandes, et al, 1997) • ↑ incidence with ↑ age • √ GBM : peak incidence at 4570 years • CVC line • ESA (erythropoiesis • Not usu applicable for Gliomas stimulating agent) • Obesity • ? Patient specific Other patient specific risks: • Cardiovascular risk factors: htn, DM, cigarette smoking, high cholesterol levels • Genetic risk factors: factor V Leiden, prothrombin gene mutation G20210A, protein C and S deficiency, and anti-thrombin deficiency Assessment/ Diagnosis S/S: • DVT “classic” calf pain, redness, tenderness, swelling • ** steroids may mask • Acute PE: dyspnea, tachypnea, and pleuritic chest pain- also apprehension, cough, syncope, and tachycardia. Dx: US, VQ scan, CXR, CT Photo by Dr. James Heilman, used with permission ©2000 by Radiological Society of North America teaching slide Schoepf U J et al. Radiology 2000;217:693-700 Peri-Op Prophylaxis Mechanical compression Photo by ME Davis, used by permission • Ruff & Posner 1983; retrospective chart review-postop glioma pts: elastic bandages verses external pneumatic compression; Incidence clots 25% vs 3% • Frim et al, 1992: Neurosurgery regimen: compression boots and low dose heparin: adding heparin sig ↓ VTE Peri-Op Prophylaxis • MacDonald, et al 2003: Unfractionated Heparin vs LMWH with pneumatic compression boots in craniotomy patients - No difference in intra-op blood loss, transfusion requirements or post-op plts counts - No difference in post-op VTE events, hemorrhage or thrombocytopenia • Pan, Tsa & Mitchell, 2009 : retrospective review of 294 GBM pts with VTE – 2 % rate ICH: “the benefits of anticoagulation therapy may outweigh the risk of ICH” Ambulatory Prophylaxis • Vena Cava Filters • prevention of PE for hi risk pts • Contraindication to anticoag • Filter does NOT prevent DVT • Anticoagulation • PROTECHT (Prophylaxis of thromboembolism during chemotherapy) Trial (Agnelli et al, 2009) • SAVE-ONCO (Agnelli, et al 2011), FRAGEM (Marraveyas, et al 2012) • PRODIGE (Prophylaxis Using Dalteparin in Glioblastoma Multiforme) Trial (Perry et al, 2010) • Meta-analysis: Aikens, Rivey & Hansen, 2013 Prophylaxis ASCO, 2007 • All hospitalized cancer patients should be considered for prophylaxis in the absence of bleeding or other comps. • Routine prophylaxis of ambulatory cancer pts is NOT recommended except pts on lenalidomide or thalidomide • Pts undergoing major surgery for malignant disease should be considered for pharmacologic prophylaxis Prophylaxis NCCN Guidelines, 2013 • All surgical oncology pts receive pharmacologic VTE prophylaxis with or without mechanical prophylaxis for duration of hospitalization • if contraindications to anticoag- mechanical prophylaxis should be used; • High risk post op patients- extended duration of prophylaxis up to 4 weeks Anticoagulation • Unfractionated heparin (UFH)converting to warfarin • Low Molecular weight Heparin (LMWH) : – Dalteparin - Fragmin® – Enoxaparain - Lovenox® – Tinzaparin - Innohep® • Factor Xa inhibitor: Fondaparinux- Arixtra® Clot Trial Treatment VTE Lee, et al, 2003 676 pts pt with active Ca and acute VTE randomized to either • LMWH (Dalteparin) 200 IU/kg/day x 1mo then ↓ 150 IU x 5months • LMWH (Dalteparin) 200 IU/kg x 5 days with transition to oral warfarin Results: LMWH only arm: 50% reduction in recurrent VTE (9 vs 17% p= .002) with no difference in rate of major bleeding (6% vs 4% p=.27) • Results repeated and confirmed (Cochrane Review) • NCCN guidelines recommend LMWH FIRST line for Ca pts Treatment VTE MSK Guidelines: Tx ADULT Acute DVT/PE: • Enoxaparin (Lovenox®) 1mg/kg SCq 12 (alternatively 1.5mg/kg SC QD) Patient Weight (kg) Enoxaparin Dose (mg) = Syringe Size Used 40-50.9 40 51-70.9 60 71-90.9 80 91-110.9 100 111-140.9 120 141-165 150 >165 Requires hematology consult Nsg Considerations- VTE • Pt/family education: – – – – – Pt risk factors, s/s VTE Promotion of activity as tolerated/ indicated Medication indication, dose, schedule, SE, self care Subcutaneous injection technique, needle disposal When to call & S/S to report • Monitor for SE, bleeding; – Special caution LMWH: renal insufficiency, obesity, LBW/elderly <50kg – Antiangiogenic therapies Anti-angiogenic therapy and Anticoagulation Limited data- mainly retrospective reviews • Nghiemphu, Green, Pope, Lai & Cloughesy, 2007 • Norden, Bartolomeo at al, 2011 “Data raises concern about the risks of full anticoagulation in bevacizumab treated pts, however both VTE and bleeding are a known risk… (from gliomas) and whether or not anticoagulation increases this risk to a clinically significant degree has yet to be shown” (Perry, 2010, pg 595) References • • • • • • • • Agnelli, G., George, D.J., Kakkar, A.K. et al (1012) Semuloparin for thromboprophylaxis in patients receiving chemotherapy for cancer NEJM 366, 601-9. Agnelli, G., Gussoni, G., Bianchi, C et al, (2009) Nadroparin for the prevention of thromboembolic events in ambulatory patients with metastatic or locally advanced solid cancer receiving chemotherapy: a randomised placebo-controlled double blind study. Lancet Oncology 10 ,943-949. Aikens, G.B., Rivey, M.P. & Hansen C.J. (2013) Primary Venous Thromboembolism Prophylaxis in ambulatory cancer patients The Annals of Pharmocology 47, 198-209 Batchelor T.T. & Byrne, T.N. (2006) Supportive care of brain tumor patients. Hematol Oncol Clin N Am 20 , 1337-1361. Brandes, A.A., Scelzi, E., Salmistraro, G. et al (1997) Incidence of risk of thromboembolism during treatment high-grade gliomas: a prospective study. EurJ cancer33, (10) 1592-96. Frim, D.M., Barker, F.G., Poletti, C.E & Hamilton A. (1992) Postoperative low-dose heparin decreases thromboembolic complications in neurosurgical patients Neurosurgery 30 (6) 830-833. Jenkins , E.O., Schiff, D., Mackmanm N. & Key, N.S. (2010) Venous thromboembolism in malignant gliomas J Thromb Haemost 8 (2) 221-227. Khorana, A.A., Kuderer, NM., Culakova, E., Lyman, G.H.& Francis, C.W. (2007) Development and validation of a predictive model for chemotherapy associated thrombosis References • Lee, A.Y., Levine, M.N., Baker, R.I. et al (2003) Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. NEJM 10;349(2):146-53. • Lyman, G.H.,et.al (2007) American Society of Clinical Oncology Guideline: recommendations for Venous Thromboembolism Prophylaxis and treatment in patients with Cancer. JOC 25( 34) 5490-5505. • Maraveyas, A., Walters, J., Roy, R. et al (2012) Gemcitabine verses gemcitabine plus dalteparin thromboprophylaxis in pancreatic cancer Eur J Canc 48, 1283-92. • Marras, L.C Geerts, W.H, & Perry, J.R (2000) The risk of venous thromboembolism is increased throughout the course of malignant glioma: an evidence based review Cancer 89 (3) 640-6. • Nghiemphu, P.L., Green, R.M., Pope, W.B., Lai, A.,& Cloughesy, T.F (2008) Safety of anticoagulation use and bevacizumab in patients with glioma Neuro-oncology 10: 355-360. • Norden, A.D., Bartolomeo, J., Tanaka, S….& Wen, P.Y (2011) Safety of concurrent bevacizumab and anticoagulation in glioma patients J Neuroonc106; 121-125 • Perry, J.R. (2010) Anticoagulation of malignant glioma patients in the era of novel antiangiogenic agents Current Opinions in Neurology 23: 592-596. References • • • • • Perry, J.R., Julian, J.A., Laperriere, N.J et al.,(2010)PRODIGE: a randomized placebocontrolled trial of dalteparin low molecular weight heparan thromboprophylaxis in patients with newly diagnosed malignant glioma J Thomb Haemost 8, 1959-65. Ruff, R. L. & Posner, J.B. (1983) Incidence and treatment of peripheral venous thrombosis in patients with glioma Annals of Neurology 13 (3) 334-336. Sartori, M.T. et al (2010) Prothrombotic state in glioblastoma multiforme: an evaluation of the procoagulant activity of circulating microparticles J Neuroncol doi 10.1007/z11060-010-0462-8 Semrad , T.J., O’Donnell, R., Wun, T., Chew, H., Harvey, D., Zhou, H & White, R. (2007) Epidemiology of venous thromboembolism in 9489 patients with malignant glioma J Neurosurg 106:601–608, Streiff, M.B (2011) Anticoagulation in the management of venous thromboembolism in the cancer patient J Thromb Thrombolysis 31; 282-294. Thank you! Any Questions? Neuro-Onc SIG Meeting I. II. III. IV. V. VI. VII. VIII. VIX. Agenda Introduction & Welcome CEU Presentation: Venous Thromboembolic Events: Care Strategies for the Neuro-Onc Patient Volunteer to take minutes: Call to order: Minutes from previous meeting: (Next slide) Approval of Minutes Discuss Sig Goals/Objectives: SIG Survey Questions: •Writing, presentations, leadership, mentoring •Virtual CME? •Do you get the newsletter/read it? • Ideas for Newsletter topics?? •would like to get involved(leave name/ email) Burning Clinical Questions/discussion