(JA)

It’s the simple things in life we forget
You hear her talkin’ but don’t hear what she said
Why do you make something so easy so complicated?
Searching for what’s right in front of your face..
- Simple Things by Usher
APPROACH TO COUGH
Jerry V. Pua MD
2 nd year Resident
Objectives
To discuss etiology, differential diagnosis and work up for children presenting with cough
To discuss approach, diagnosis, management, recommendations and prevention of B. pertussis infection
General Data
A.E.
6 month old, Female
Filipino, Catholic
Brgy. Batasan Hills, Quezon City
Consulted at ER last June 15, 2013
Informant: Grandmother
Reliability: 80%
Cough – 2 weeks duration
Chief Complaint
History of Present Illness
2 weeks
PTA
• Non productive cough
• No fever nor other associated symptoms
• No consult done
5 days PTA
• Persistence of recurring bouts of cough
• No other associated symptoms
• Consulted LHC – Carbocisteine and
Amoxicillin (40mkday)
History of Present Illness
3 days PTA
• Persistence of continous non productive cough followed by facial cyanosis
• Difficulty breathing – alar flaring, tachypnea, ‘seesaw’ breathing
Few hours
PTA
• Persistence of symptoms prompted consult at Local Clinic
• A> Bronchopneumonia rule out Pertussis
• Advised consult at a tertiary institution
Review of Systems
Decrease appetite
No failure to thrive, feeding interruption
No skin lesions
No diaphoresis, no fainting spells
No vomiting, no diarrhea nor constipation
No pallor
No facial redness during bouts of cough
No convulsion
No limitation of movements
No bleeding manifestations
Family History
(+) cough (+)
(+)
No heredo-familial disease on both sides of the family
Birth and Maternal History
Born to 39 year old G5P4 (4014) non smoker, non alcoholic beverage drinker mother
No pre natal check up, denies maternal illness
Multivitamins, Ferrous Sulfate intake
Delivered Full term via NSD at home assisted by traditional birth attendant
No feto-maternal complication during and after the delivery
Immunization History
No immunization received
Nutritional History
Milk Formula – since birth
No milk formula intolerance
Complimentary feeding – 6 months old
No interrupted feeding
No feeding problems
Growth and Development
Motor
Head control – 2 mos. rolls over – 4 mos. sits with support –
6 mos.
Language
Imitates sounds – 5mos
Daily Living
Put anything at the mouth – 4 mos.
Social/Adaptive
Social smile – 2 mos. plays with caregiver – 6 mos
Past Medical History
No routine check up
No previous hospitalization
No previous surgical intervention done.
No allergies
Physical Examination
Awake, irritable, in mild respiratory distress. Well hydrated.
Weight: 6 kg (z score below 0 )
Height: 65 cm (z score 0 )
BP 80/50 HR 122
RR 38 T 37.1
Skin: Warm, Moist, No rashes or other dermatosis.
No cyanosis.
Physical Examination
HEENT: Normocephalic. Aniceteric sclera; pink palpebral conjunctivae; no eye discharge
(+) intermittent alar flaring. No nasal discharge nor bleeding. No tragal tenderness, no aural discharge
Non hyperemic posterior pharyngeal wall, no exudates, uvula midline
(+) cervical lympadenopathy, bilateral
Chest and Lungs: No chest deformity nor skin lesions at the chest. Symmetrical chest expansion, (+) subcostal and intercostals retractions (+) crackles on both lung fields
Physical Examination
Heart: Adynamic precordium, Apex beat at 4 th ICS
LMCL, normal rate regular rhythm, no murmur
Abdomen: Globular, No visible veins. Normoactive bowel sounds. Soft, non tender, no organomegaly.
Genitalia: Grossly female
Extremities: No preferential movement. Pulses on all extremities are full and equal. No clubbing,
cyanosis of fingers or toes. CRT <2 seconds. No deformities.
Neurologic Examination
Mental Status: Awake, irritable. GCS 15
Cranial Nerves: Intact
Motor: Good muscle tone, no fasciculation or atrophy, no involuntary movement. MMT 5/5 on all extremities. DTR’s 2++
Sensory: No deficit. No babinski or clonus.
Cerebellar: No nystagmus
Meningeal signs: No Kernig’s, No Brudzinski, No nuchal rigidity
BRONCHOPNEUMONIA
RULE OUT PERTUSSIS
NO STUNTING NO WASTING
Admitting Impression
SYMPTOMS, SIGN, OR LABORATORY
FINDINGS PATHOGNOMONIC OF A
DISEASE
Approach to Diagnosis
COUGH
Most common symptom presenting to medical practitioners
Cough is a forced expulsive maneuver, usually against a closed glottis
Sound of a cough is due to vibration of larger airways and laryngeal structures during turbulent flow in expiration
Cough quality in children: a comparison of subjective vs. bronchoscopic findings
Anne Bernadette Chang, et. al
Dept of Paediatrics & Child Health, University of Queensland
Dept Respiratory Medicine, Royal Children's Hospital, Brisbane
COUGH
Estimating the duration of cough is the first step in narrowing the list of possible diagnoses
THE DIAGNOSIS AND TREATMENT OF COUGH
RICHARDS. IRWIN, M.D.,AND J. MARK MADISON, M.D.
The New England Journal of Medicine
Types of Cough (Duration)
Acute Cough -- a recent onset of cough lasting <3 weeks
Subacute Cough (Prolonged acute cough) -- cough slowly resolving over a 3–8-week period
Chronic Cough -- A cough lasting >8 weeks
Recurrent Cough -- cough without a cold is taken as repeated (>2/year) cough episodes, apart from those associated with colds, that each last more than 7–14 days
Recommendations for the assessment and management of cough in children
M D Shields, A Bush, M L Everard, S McKenzie, R Primhak, on behalf of the
British Thoracic Society Cough Guideline Group
ACUTE COUGH
Cough lasting for a maximum of 3 weeks
Common caused: URTI, acute bronchitis or tracheobronchitis (bacterial or viral)
Such infections is usually self limited and subsides within one to two weeks along the clearing of the infection
No targets or reliable measures to predict the duration of cough at its onset, also to predict which will persist into sub acute or chronic cough
COUGH MANAGEMENT: A Practical Approach
F. De Blasio, et. al
COUGH MANAGEMENT: A Practical Approach
F. De Blasio, et. al
COUGH MANAGEMENT: A Practical Approach
F. De Blasio, et. al
Types of Cough (Causes)
Specific Cough -- one in which there is a clearly identifiable cause
Non specific isolated Cough -- typically have a persistent dry cough, no other respiratory symptoms, well with no signs of chronic lung disease and have a normal chest radiograph
Post viral Cough -- cough originally starting with an upper respiratory tract infection but lasting <3 weeks
Recommendations for the assessment and management of cough in children
M D Shields, A Bush, M L Everard, S McKenzie, R Primhak, on behalf of the
British Thoracic Society Cough Guideline Group
Types of Cough (Quality)
Classic Recognizable Cough
Certain cough characteristics classically taught to point to specific etiologies
Dry Cough
Wet Cough
Cough in children: definitions and clinical evaluation
Position statement of the Thoracic Society of Australia and New Zealand
Salient Features
6 months old
2 weeks history of cough
No fever
Cyanosis at bouts of cough
Difficulty of breathing
Siblings with cough
No immunization received
In mild respiratory distress
Intermittent alar flaring
Intercostal and subcostal retractions
Crackles on both lung fields
Course at the Ward
Patient: A.E.
6 months old, Female
Working Impression:
Bronchopneumonia
Rule out Pertussis
1
st
Hospital Day
Diagnostics
Arterial Blood Gas pH 7.24 pCO2 26 pO2 179 O2sat 99
HCO3 11.1 BE - 14.7
CBC w/ PC
Hgb 37.7 Hct
WBC 35.5 Seg
0.42
21
Lympho 79 Platelet 647
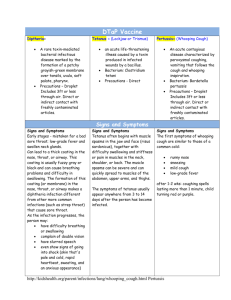
Case Definitions: Pertussis (WHO)
Cough lasting at least 2 wk with at least 1 of the following symptoms:
paroxysms of coughing
inspiratory whooping
posttussive vomiting (ie, vomiting immediately after coughing)
Clinical case: a case that meets the clinical definition, but is not laboratoryconfirmed
Laboratory-confirmed case: a case that meets the clinical case definition and is laboratory-confirmed
Clinical Definitions of Pertussis: Summary of a Global Pertussis Initiative
Roundtable Meeting, February 2011
Clinical Definitions: Pertussis (CDC)
Cough illness lasting ≥ 2 weeks with 1 of the following without apparent cause:
Paroxysms of coughing
Inspiratory “whoop”
Posttussive vomiting
Probable case: symptoms, absence of laboratory confirmation and epidemiologic linkage to a laboratory-confirmed case of pertussis
Confirmed case: symptoms + > 1 following – PCR positive for pertussis or contact with laboratory-confirmed case of pertussis
Clinical Definitions of Pertussis: Summary of a Global Pertussis Initiative
Roundtable Meeting, February 2011
Diagnostics
Common laboratory diagnostic methods:
Culture – gold standard
Direct antigen detection PCR
Direct fluorescent antibody (DFA) testing
Serologic demonstration enzyme-linked immunosorbent assay (ELISA) or Western blot with various B. pertussis antigens and agglutination
Measuring an increase in titers between acute and convalescence phase serum specimens or high single serum antibody values
Defining Pertussis Epidemiology
Clinical, Microbiologic and Serologic Perspectives
James D. Cherry, MD, et al Pediatr Infect Dis J 2005
Diagnostics: Serologic Testing
Proper performance of culture, PCR and ELISA to measure increases or decreases in IgG and IgA antibody titers to
Pertussis Toxin in paired serum samples, the sensitivity and specificity of the laboratory diagnosis of B. pertussis infection
The greatest sensitivity is obtained when culture, PCR and serologic testing are all performed on individuals with cough illness
Defining Pertussis Epidemiology
Clinical, Microbiologic and Serologic Perspectives
James D. Cherry, MD, et al Pediatr Infect Dis J 2005
Pertussis PCR
Key factors for the successful application of PCR in the diagnosis of infection by Bordetella spp.:
Sample collection and processing
DNA purification
Primer selection
Amplification conditions
PCR as a diagnostic tool has the advantage of a much higher sensitivity compared with conventional culture
Defining Pertussis Epidemiology
Clinical, Microbiologic and Serologic Perspectives
James D. Cherry, MD, et al Pediatr Infect Dis J 2005
Pertussis: PCR
A 2.6-fold increase in detection of B. pertussis using PCR
compared with culture
PCR results were compared with serologic diagnosis;
PCR had a sensitivity of 61% and a specificity of 88%
Patients with symptoms meeting the CDC clinical case definition for pertussis and who had a specimen positive by PCR or DFA were considered to have true B. pertussis infections
Defining Pertussis Epidemiology
Clinical, Microbiologic and Serologic Perspectives
James D. Cherry, MD, et al Pediatr Infect Dis J 2005
2
nd
Hospital Day
Diagnostic
Referred to Infection Control Committee
Blood CS
Nasopharyngeal Pertussis PCR
2D Echo with PAP
Complete Blood Counts
Hemoglobin
Hematocrit
WBC Count
Diff. Count
Segmenter
Lymphocytes
Monocytes
Platelet
06/15/13 06/16/13 06/17/13 06/18/13 06/20/13
137.7
125.1
126.2
131.4
140.3
0.42
35.5
0.38
27.5
0.38
25.9
0.40
19.2
0.43
16.8
21
79
647
14
72
10
523
16
65
15
537
21
62
14
539
31
63
06
465
Diagnotics: Complete Blood Count
A total count of ≥ 20,000 WBCs/mm3 with ≥
10,000 lymphocytes/mm3 in a young infant with coryza, cough, apnea or other respiratory distress is indicative of B. pertussis infection
A total count of ≥ 30,000 WBCs/mm3 is cause for concern and the rapidity of the WBC count rise is also an important indicator of worsening condition
Pertussis in Young Infants – Guidance for Clinicians
James D. Cherry MD, et. al. May 2010
Microbiology
Blood Culture and Sensitivity:
No growth for 5 days of incubation
Nasopharyngeal Bordetella pertussis
Polymerase Chain Reaction
POSITIVE for Bordetella pertussis DNA
PERTUSSIS
BRONCHOPNEUMONIA
NO STUNTING NO WASTING
Final Diagnosis
Pertussis
Acute respiratory infection caused by Bordetella pertussis
‘intense cough’
Extremely contagious -- attack rates as high as
100% in susceptible individuals exposed to aerosol droplets at close range
Bordetella pertussis
Tiny, fastidious, gram-negative coccobacilli that colonize only ciliated epithelium
Expresses pertussis toxin (PT), the major virulence protein
After aerosol acquisition, pertussis organism attaches to ciliated respiratory epithelial cells
Tracheal cytotoxin, adenylate cyclase, and PT appear to inhibit clearance of organisms
Responsible for the local epithelial damage
Epidemiology
Worldwide, pertussis is a significant cause of infectious mortality
20 to 40 million cases
200,000 to 400,000 death per years
Most of cases and deaths occur in infancy
WHO. Pertussis vaccines. Wkly Epidemiol Rec. 1999;74:137 –143
Epidemiology
Philippine Pediatric Society Registry
99 out of 1935660 cases
Philippine Children’s Medical Center
32 cases: Total probable and confirmed pertussis cases admitted from JANUARY-JUNE 2013
Source of Infection
Rate of subclinical infection is as high as 80%
Coughing adolescents and adults -- major reservoir for B. pertussis -- usual sources of infection for infants and children
Household contact with infected adolescent and
adults – major source of pertussis infection in not fully immunized infants
Infant Pertussis and Household Transmission n Korea.
The Korean Academy of Medical Sciences.
Mode of Transmission
Stages of Pertussis Infection
Catarrhal stage (1-2 wk) begins insidiously after an incubation period (3-12 days)
Paroxysmal stage (2-6 wk) onset marks by coughing
Cough begins as a dry, intermittent, irritative hack and evolves into the inexorable paroxysms
Post-tussive emesis is common, and exhaustion is universal.
Convalescent stage (≥2 wk), the number, severity, and duration of cough episodes diminishes
Stages of Pertussis Infection
Pertussis in Young Infants
Catarrhal stage -- characterized by excessive sneezing or
“throat clearing” -- adherence of organism in the ciliated epithelium throughout the respiratory tract – tissue necrosis, production of mucus, and inflammatory cell response
Paroxysmal stage – atypical
Acute life-threatening episode is common
Spells of cough leading to cyanosis or bradycardia and limpness as well as apnea
Post-tussive vomiting is common
“whoop cough” is rarely present in very young infant
Review: Age-Specific Presentation and Burden of Pertussis by Sarah Long M.D.
1
st -
2
nd
Hospital Day
Management
Isolation
D5LR (mild)
O2 at 10Lpm
Medications:
Ampicillin (100)
Erythromycin (40) ---- Azithromycin (10)
Salbutamol nebulization every 4 hours
NPO
Goals of hospitalization
Assess progression of disease and likelihood of lifethreatening events at peak of disease
Prevent or treat complications
Educate parents in the natural history of the disease and in care that will be given at home
Goals of therapy
Limit the number of paroxysms
Observe the severity of the cough
Provide assistance when necessary
Maximize nutrition, rest, and recovery without sequelae
Age
Medications
Primary Agents
Azithromycin
<1 mo 10 mg/kg/day in a single dose for 5 days
Alternate Agents
Erythromycin
(Infantile hypertrophic pyloric stenosis)
40-50 mg/kg/day in 4 divided doses for 14 days
Clarithro
Not recommended
(safety data unavailable)
TMP-SMZ
Contraindicated for infants aged <2 mo (risk for kernicterus)
1-5 mo 10 mg/kg/day in a single dose for 5 days
40-50 mg/kg/day in 4 divided doses for 14 days
15 mg/kg/d in 2 divided doses for 7 days
Contraindicated at age
<2 mo
For infants aged ≥2 mo:
TMP 8mg/kg/day plus
SMZ 40 mg/kg/day in
2 divided doses for 14 days
Infants aged
≥6 mo and child
10 mg/kg in a single dose on day 1
(maximum 500 mg), then 5 mg/kg/day
(maximum 250 mg) on days 2-5
40-50 mg/kg/day
(maximum 2 g/day) in
4 divided doses for 14 days
15 mg/kg/d in 2 divided doses
(maximum
1 g/day) for
7 days
TMP 8 mg/kg/day plus
SMZ 40 mg/kg/day in
2 divided doses for 14 days
Pertussis Complications in Young Infants
Life-threatening complications are most common in infants younger than 3 months
Respiratory tract complications: apnea, bacterial pneumonia, and pulmonary hypertension
Secondary bacterial pneumonia – leading identified cause of pertussis-related infection
Review: Age-Specific Presentation and Burden of Pertussis by Sarah Long M.D.
Pertussis Complications in Young Infants
Respiratory Failure with Pertussis may stem from complications of Pneumonia, Pulmonary
Hypertension, and Apnea
Apnea – due to failure of self-rescue breathing at the end of a paroxysm of coughing or profound vagal stimulation
Infants intubated due to respiratory failure secondary to apnea have better prognosis than those intubated due to pneumonia or pulmonary hypertension
Review: Age-Specific Presentation and Burden of Pertussis by Sarah Long M.D.
Pertussis Complications in Young Infants
Severe Bordetella pertussis consist of constellation of bronchopneumonia, extreme leukocytosis, refractory hypoxemia, and pulmonary hypertension
White blood cell counts >100 000 in the setting of
B. pertussis pneumonia associated with increase mortality
Pertussis Pneumonia, Hypoxemia, Hyperleukocytosis, and Pulmonary Hypertension:
Improvement in Oxygenation After a Double Volume Exchange Transfusion
Michael J. Romano, et. al. Pediatrics 2004
Pertussis: Proposed Pathologic Course
Infection of tracheal epithelium with
Bordetella pertussis
Ciliostasis, epithelial damage and compromised mucociliary clearance apnea
Pulmonary Infection
Necrotizing bronchopneumonia
Toxin mediated leukocytosis hypoxemia
ARDS
Increase whole blood mass
Pulmonary vasoconstriction Increase vascular resistance
PULMONARY HYPERTENSION
Cardiac Failure and Shock
Pathology and Pathogenesis of Fatal
Bordetella pertussis Infection in Infants
Christopher D. Paddock, et. al.
3
rd
-5
th
Hospital Day
The rest of hospital stay patient completed her antibiotics.
O2 supplementation was titrated down and eventually discontinued.
Patient discharged well and stable.
Indications for ICU referral
Infants less than or equal 3 months old with clinical deterioration
White Cell Count more than or equal to 30, 000 or rapidly rising in count (>10,000 in 6 hours)
Respiratory failure or frequent apnea
Progressive pneumonic changes in CXR
Persistent tachycardia/ cardiovascular instability
Neurological symptoms including seizure
South Thames Retrieval Service Guideline
ICU care
Apnea, pneumonia, and seizures are the most common presenting symptoms requiring ICU care
Leukocytes aggregate within the pulmonary circulation and form a mechanical obstruction to transpulmonary blood flow with the result being severe hypoxemia and pulmonary hypertension
Cardiac failure associated with critical pertussis is likely right sided heart failure secondary to the pulmonary hypertension
Double Volume Exchange Transfusion
Multiple authors have reported double volume exchange transfusion as an effective therapy for the pulmonary hypertension, and secondarily the hypoxemia and cardiac failure
Technique of double volume exchange utilized is the same as performed for the newborn with hyperbilirubinemia
Hypomagnesemia and especially hypocalcemia may occur thus recommended routine calcium supplementation
Chen H, Lee M, Tsao L. Exchange Transfusion Using Peripheral Vessels Is Safe and Effective in
Newborn Infants. Pediatrics 2008
Indications for DVET
White cell count more than or equal to 30,000 and rapidly rising count
White cell count more than or equal to 30, 000 with pneumonia or hemodynamic instability
White cell count more than or equal 50,000
South Thames Retrieval Service Guideline
Studies shows…
Appearance of respiratory symptoms paralleled the rise in leukocyte count
Temporal relationship between the initiation of exchange transfusion and improvement in oxygenation
Pertussis Pneumonia, Hypoxemia, Hyperleukocytosis, and Pulmonary Hypertension:
Improvement in Oxygenation After a Double Volume Exchange Transfusion
Michael J. Romano, et. al. Pediatrics 2004
Pertussis Pneumonia, Hypoxemia, Hyperleukocytosis, and Pulmonary Hypertension:
Improvement in Oxygenation After a Double Volume Exchange Transfusion
Michael J. Romano, et. al. Pediatrics 2004
Criteria for Hospital Discharge
Over a 48-hr period disease severity is unchanged or diminished
No intervention is required during paroxysms
Nutrition is adequate
No complication has occurred
Parents are adequately prepared for care at home
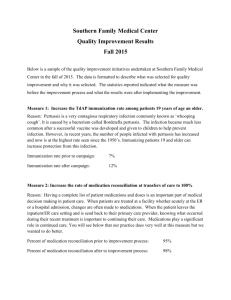
Prevention: Vaccination
Efficacy of the vaccine in reducing disease severity was 48% among children vaccinated with 3 doses of whole-cell (67%) or acellular (32%)
Pertussis vaccination substantially decrease the severity of breakthrough disease in vaccinated children (3 doses) compared to unvaccinated children
Unvaccinated children twice likely to have severe disease than vaccinated children
Effects of Pertussis vaccination on Disease: Vaccine Efficacy in Reducing Clinical Severity
Preziosi, Marie-Pierre, et.al. Clinical Infectious Disease 2003
Prevention: Vaccination
DTaP (Diphtheria, tetenus toxoid and acellular
Pertussis)
contain inactivated PT and 2 or more other bacterial components (FHA, Pn, and Fim 2 and 3)
4 doses during the 1 st 2 years of life
2,4,6 and 15-18 months
5th dose of DTaP recommended for children at 4-6 yr of age
Prevention: Vaccination
Tdap (Tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis vaccine, adsorbed)
Preferred age for Tdap vaccination is 11-12 yr
Pregnant adolescents who are in their 2nd or 3rd trimester
All adolescents 11-18 yr of age who received Td, but not Tdap, should receive a single dose of Tdap to provide protection against pertussis
Vaccination of women during pregnancy and newborns
Timing of maternal Tdap immunization is important
– administered during the third trimester to have maternal pertussis antigen-specific IgG levels at their peak
Immunization with DTaP or aP vaccines is not recommended in newborns -- controversial
Pertussis re-emergence in the post-vaccination era
Chiappini et al. BioMedCentral Infectious Disease 2013
Cocooning strategy
Providing indirect protection to infants who are too young to be immunized or protected by vaccine through immunization of their parents and other family members, caregivers and close contacts
Pertussis re-emergence in the post-vaccination era
Chiappini et al. BioMedCentral Infectious Disease 2013
Vaccination of preschool and adolescent
Contributes to increase herd immunity
Reduce transmission of pertussis to susceptible population
Reduce reservoir of pertussis within population and indirectly prevent pertussis case in infants and young children
Pertussis re-emergence in the post-vaccination era
Chiappini et al. BioMedCentral Infectious Disease 2013
Immunization of health-care workers
Pertussis among health-care personnel has been reported to be 1.7 times higher than the general population
Health-care personnel who have direct contact with patients should receive single dose of TdaP as soon as feasible, if they have not previously received
TdaP
Pertussis re-emergence in the post-vaccination era
Chiappini et al. BioMedCentral Infectious Disease 2013
Updates
Patient follow up at OPD – well, active
Received her first dose of DPT, OPV, and
Hepatitis B
Relatives were educated regarding the importance of immunization as well as proper hygiene to stop the vicious cycle of transmission
Summary
A case of 6 month old unimmunized infant who presented with subacute cough with paroxysms, who after a nasopharyngeal swab PCR was confirmed with Bordetella pertussis
Started on Azithromycin per orem and eventually discharged well and stable
Recommendations for management of pertussis
Emphasized the importance of immunization on preventing vicious transmission cycle