Inhalation Injury - University of Colorado Denver

Inhalation Injury
Arek Wiktor M.D.
Burn Fellow
University of Colorado Hospital
Outline
Background
Smoke
Pathophysiology
Diagnosis
Treatment
Specific Lethal Compounds http://spanishlakefd.com/firealarms/
Learning Objectives
Describe the pathophysiology of inhalation injury
How is inhalation injury diagnosed?
What adjunctive measures are used to treat inhalation injury?
What is the treatment for carbon monoxide and cyanide poisoning?
A Sunday afternoon stroll thru the fire… http://www.aeromedix.com/product-exec/parent_id/1/category_id/12/product_id/1074/nm/Safe_Escape_Smoke_Hood
Epidemiology
15-30% of burn admissions have inhalation injury
Independent predictor of mortality, ↑ by 20%
Increases pneumonia risk
Leading diagnosis of those hospitalized and treated on 9/11, World Trade Center attack
Anatomic Classification
Upper airway
Lower airway
Systemic toxicity http://www.monroecc.edu/depts/pstc/backup/parasan4.htm
SMOKE
Variable, changes with time burning
Toxic gases and low ambient oxygen
Ingredients:
Aldehydes (formaldehyde, acrolein), ammonia, hydrogen sulfide, sulfur dioxide, hydrogen chloride, hydrogen fluoride, phosgene, nitrogen dioxide, organic nitriles
Particulate matter
Prien et al. Burns 1988; 14:451-460
Pathophysiology
Cilia loss, respiratory epithelial sloughing
Neutrophilic infiltration
Atelectasis, occlusion by debris/edema
Pseudomembranes
Bacterial colonization at 72 hrs
Hubbard et al. J Trauma 1991; 31:1477-1486
Bartley et al.
Drug Design, Development and
Therapy. 2008; 2: 9–16.
Secondary Lung Injury
Unilateral smoke inhalation damages contralateral lung
Immune response, increased permeability
Oxygen-derived free radicals
NO mediated damage (chemotactic factor neuts)
Eiscosanoids (TXA2→TXB2)
Reduced phagocytosis in macrophages
Systemic Effects
Larger fluid resuscitation (2→5cc/kg/%)
Additive effect to burns
12% pts inhalation injury alone require intubation *
62% pts burn + inhalation injury intubated *
Clark et al. J Burn Care Rehabilitation, 1990; 11:121-134
Miller et al. Journal of Burn Care Research. 2009; 30(2) 249-256
Diagnosis
Clinical findings:
Facial burns (96%)
Wheezing (47%)
Carbonaceous sputum (39%)
Rales (35%)
Dyspnea (27%)
Hoarsness (26%)
Tachypnea (26%)
Cough (26%)
Cough and hypersecretion (26%)
DiVincenti et al. Journal of Trauma, 1971; 11:109-117
NO ONE FINDING IS
SUFFICIENTLY SENSITIVE
OR SPECIFIC!
Must use clinical judgment!
Tools for Diagnosis
Bronchoscopy
Pulmonary function testing
Xenon 133 lung scan
Grades of Inhalation Injury
Endorf and Gamelli. Journal of Burn Care and Research. 2007; 28:80-83
Treatments
Airway Control
Chest physiotherapy
Suctioning
Therapeutic bronchoscopy
Ventilatory strategies
Pharmacologic adjuncts
Treatment
Control the Airway!!!
≥ 40% burn
Transport http://www.burnsurgery.com/Betaweb/Modules/initial/bsinitialsec2.htm
Ventilator Strategies
Airway pressure release ventilation (APRV)
Intrapulmonary percussive ventilation (IPV)
High-frequency percussive ventilation (HFPV)
High frequency oscillatory ventilation (HFOV)
Single center, prospective randomized trial 2006-2009
387 pts screened
31 pts HFPV, 31 pts LTV (ARDSnet)
Chung et al. CCM; 2010: 38(10) 1970-1977
Results
No significant difference in mortality or ventilator free days
Significant difference in “Rescue Therapy”
Results
No significant difference in mortality or ventilator free days
Significant difference in “Rescue Therapy”
P/F ratio vs Ventilator Mode
Chung et al. CCM; 2010: 38(10) 1970-1977
Study Conclusions
Study stopped for safety concerns in LTV group
Gas exchange goals met in all HFPV pts, and not in 1/3 of LTV pts
Trend for less barotrauma, less VAP, less sedation
“Strict application of LTV may be suboptimal in the burn population”
Pharmacologic Intervention
Bartley et al. Drug Design, Development and Therapy. 2008; 2: 9–16.
Pharmacologic Intervention
Bartley et al. Drug Design, Development and Therapy. 2008; 2: 9–16.
Airway Obstructive Casts
Mucus secretions
Denuded airway epithelial cells
Inflammatory cells
Fibrin
-Solidifies airway content
Several studies shown reduction in size of casts with fibrinolytic agents (tPA)
Casts
Enkhbaatar et al., 2007
Theory Behind Inhaled Heparin
Animals with Burn + ARDS have decreased levels of antithrombin in plasma and BAL specimens
Heparin potentiates antithrombin by 2000x
Prevention of fibrin deposition in lungs
Heparin inhibits antihrombin’s antiinflammatory effect - ? systemic rhAT ?
Shriners Protocol
Since 1990 (560+ patients treated)
Mlcak RP et al. Burns, 2007;33:2-13
Evidence (Pro)
Desai et al. 1998
Pediatric burns (90 pts total)
1985-1989 (43) vs 1990-1994 (47pts)
↓ reintubation, atelectasis, and mortality
Miller et al. 2009
30 patients over 5 years, retrospective review
Tx 10,000 units heparin, 20% NA, 0.5 ml AS q4 hrs
Survival benefit, improved LIS scores, compliance
Number needed to treat 2.73
Evidence (Con)
Holt et al. 2008
Retrospective review 1999-2005, 150 pts total
Burn size, LOS, time on vent, mortality SAME
Only 68% pts had bronchoscopy,
Attending discretion which treatment to use
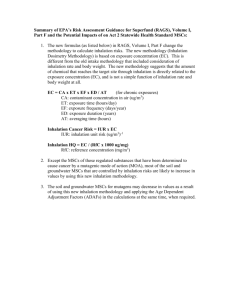
TOXIC GASES
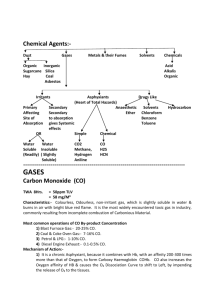
Carbon Monoxide (CO)
CO from incomplete combustion
CO + Hb → COHb
(affinity 200-250x)
LEFT shift of oxy-Hb curve (Haldane effect)
CO binding to intracellular cytochromes and metalloproteins (myoglobin)
“Two compartment” pharmacokinetics
Animal experiment 64% COHb transfusion
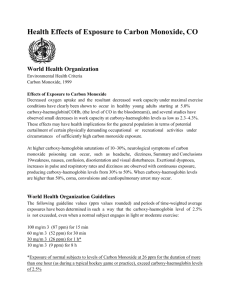
CO Toxicity Symptoms
“Cherry-red lips, cyanosis, retinal hemorrhage”rare
CNS and Cardiovascular
↑ RR, ↑HR, dysrhythmias, MI, ↓BP, coma, seizures
Delayed neuropsychiatric syndrome (3-240d)
Cognitive/personality changes/parkinsonianism
Spontaneous resolution
Signs and Symptoms
Weaver LK. N Engl J Med 2009;360:1217-25.
CO Toxicity Diagnosis
Pulse oximetry false
HIGH SpO
2
Need cooximetry direct measurement of
COHb
Older ABG analyzers (estimate off dissolved PO
2
)
MRI – lesions globus pallidus/basal ganglia/deep white matter
COHb
%
Symptoms
0-5 Normal
15-20 Headache, confusion, fatigue
20-40 Hallucination, vision
Δ’s
40-60 Combative, coma
60 + Cardiopulmonary arrest
CO Toxicity Diagnosis
Pulse oximetry false
HIGH SpO
2
Need cooximetry direct measurement of
COHb
Older ABG analyzers (estimate off dissolved PO
2
)
MRI – lesions globus pallidus/basal ganglia/deep white matter
COHb
%
Symptoms
0-5 Normal
15-20 Headache, confusion, fatigue
20-40 Hallucination, vision
Δ’s
40-60 Combative, coma
60 + Cardiopulmonary arrest
CO Toxicity Treatment
OXYGEN
Half-life COHb (min)
RA
1ATM
Male 240
Female 168
100%
O
2
47
100% O
2
2.5 ATM
22
33 15
Carbogen – normobaric, normocapnic, hyperventilation (4.5-
4.8% CO
2
)
Hyperbaric oxygen???
Cyanide (CN)
Combustion of synthetics (plastics, foam, varnish, paints, wool, silk)
Binds to cytochrome c oxidase – dose dependent
Uncouple mitochondria
Aerobic → anaerobic = Lactic acid
Half-life 1-3 hours
CN Toxicity Symptoms
Dyspnea
Tachypnea
Vomiting
Bradycardia
Hypotension
Giddiness/Coma/Siezures
Death
* The smell of bitter almonds on the breath suggests exposure
(cannot be detected by 60% of the population)
CN Toxicity Diagnosis
No rapid assay
High lactate (>10mmol/L) ( s/s, 87%/94%)
Metabolic acidosis
Elevated mixed venous saturation (<10% a-v) difference
High index of suspicion
** Also get: COHb and Methemoglobin levels
CN Treatment
Cyanokit (Hydroxocobalamin)
70mg/kg dose (5g vials)
Combines with cyanide to from cyanocobalamin (Vit B12)
Red membranes/urine
Hypertension, Anaphylaxis
5% increase COHb, interfere with HD
LFTs/Cr/Fe levels
Cyanide Antidote Kit (CAK)
Amyl nitrite pearls, sodium nitrite, and sodium thiosulfate
Amyl nitrate and sodium nitrate induce methemoglobin
Methemoglobin+cyanide→releases cyanide from CC
Sodium thiosulfate enhances cyandide→thiocynate→renal excretion
Avoid nitrate portion in pts with inhalation injury
(COHb >10%)
Vasodilation and hypotension
Acquired Methemolgobinemia
NO2, NO, benzene gases → oxidation of iron
Fe 2+ → Fe 3+
Shift curve to LEFT
Blood “Chocolate brown color”
Normal PaO2, pulse ox >85%
Tx: Methylene blue (1-2 mg/kg Q 30-60min)
Final Thoughts
Inhalation injury is bad
Support the airway
Frequent bronchoscopy and monitoring
Different ventilatory strategies
Adjunctive measures need further investigation
The Toilet Snorkel http://www.icbe.org/2006/01/18/the-toilet-snorkel/
Thank You!
Learning Objectives
Describe the pathophysiology of inhalation injury
How is inhalation injury diagnosed?
What adjunctive measures are used to treat inhalation injury?
What is the treatment for carbon monoxide and cyanide poisoning?