luka bakar,listrik dan petir
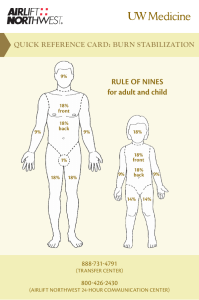
advertisement

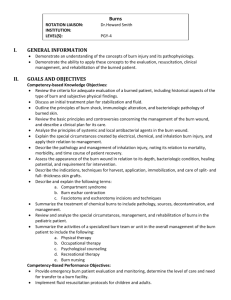
PENATALAKSANAAN AWAL KEGAWAT DARURATAN BEDAH: LUKA BAKAR,LISTRIK DAN PETIR Dr. DEDDY SAPUTRA SpBP-RE FK Unand/RSUP dr M Djamil PADANG LB: Injuri / kerusakan jaringan kulit & jaringan tubuh yang disebabkan trauma thermal. Penyebab: Api, Air panas, Zat kimia, Listrik, Petir, Ledakan dan Radiasi. MORBIDITAS & MORTALITAS: 1. Penyebab dan Lama kontak. 2. Sudah terjadi sejak fase awal LB. 2 Initial Assessment • • • • • Airway Breathing Circulation Disability Exposure • Initial burn treatment: remove burn source Prinsip Penatalaksanaan LB: Menjamin: Restorasi ABCDE • Airway dan Breathing bebas. • Perfusi normal. • Keseimbangan cairan & elektrolit. • Suhu tubuh Normal. 4 Airway & Breathing • Inhalation Injury ~7% of patients HX: closed space fire, meth lab explosion, or petroleum product combustion Upper airway injury: acute mortality • facial/intraoral burns, naso/oropharyngeal soot, sore throat, abnormal phonation, stridor Lower airway injury: delayed mortality • dyspnea, wheezing, carbonaceous sputum, COHb, PaO2/FiO2 • bronchoscopy +/• Intubate EARLY!!! Orotracheal • Surgical airway Airway disturbance Circulation • Typically burns 20% require IVF resuscitation • Resuscitate w/ kristaloid. Adult(Baxter/Parkland Formula) = 4 cc/ kg/ % burn • 1/2 over 1st 8 hr from time of burn • 1/2 over subsequent 16 hr Child (<20 kg) 3 cc/kg/% burn + D5 Goal = UOP of 30 cc/hr (1 cc/kg/hr in kids) Calculate burn size (%) • Burn depth Superficial Partial-thickness (PT) Full-thickness (FT) Indeterminate • Only partial-thickness (2nd degree), indeterminate, & full-thickness (≥3rd degree) injuries: count towards %TBSA 3 Zones of Thermal Injury Hyperemia Stasis Coagulation Burn Depth “Superficial” • Formerly “1st-degree” • • • • • Essentially a sunburn Pink Painful NO blisters Will heal in < 1 week “Partial-thickness” • Formerly “2nddegree” • • • • • Pink Moist Exquisitely painful Blistered Typically heals in < 23 weeks “Full-thickness” • Formerly “3rddegree” • • • • • Dry Leathery White to charred Insensate Will require E&G “Indeterminate” • Unsure as to whether PT or FT • Observe for conversion b/t days 3-7 • May or may not require E&G • Can unpredictably increase LOS Calculate burn size • Estimate %TBSA Palmar surface of pts hand = 1% TBSA Age-appropriate diagrams (e.g.- Berkow) Rule of Nines The Rule of Nines and Lund–Browder Charts Orgill D. N Engl J Med 2009;360:893901 17 Disability (from other injuries) • Primary & secondary surveys are important!!! • R/O non-thermal trauma … ~5% have concomitant non-thermal injury • Management of non-thermal trauma typically supercedes burn management, except for the resuscitation. Everything else • Vascular access: PIV is preferable • Analgesia = IV opiates • Conservative & judicious sedatives, prn only • Wood’s lamp eye exam for flash burns to face • Escharotomies • Early enteral nutrition (≥ 20% TBSA) Escharotomies Indications • Circumferential FT extremity burns with threatened distal tissue Diminished or absent distal pulses via doppler Any S/S of compartment syndrome. • Circumferential FT thoracic burn (Breathing disturbance) Elevated PIP or Pplateau Worsening oxygenation or ventilation Escharotomy ELECTRICAL INJURY • Zeus, the ruler of the ancient Greek gods, was characteristically depicted holding thunderbolts,which he used as warning or punishment against those who disobeyed him. • The first electrical fatality recorded in France in 1879 Shock Severity • Severity of the shock depends on: Path of current through the body Amount of current flowing through the body (amps) Duration of the shocking current through the body, • LOW VOLTAGE DOES NOT MEAN LOW HAZARD 24 PRINCIPLES OF ELECTRICITY • Electricity is the flow of electrons (the negatively charged outer particles of an atom) through a conductor. • when the electrons flow away from this object through a conductor, they create an electric current, which is measured in Amperes (I). • The force that causes the electrons to flow is the voltage, and it is measured in Volts (V). • Anything that impedes the flow of electrons through a conductor creates resistance, which is measured in Ohms (R). Electrical Injuries Factors Determining Severity OHM’S LAW: i = V / R 1. 2. 3. V = voltage i = current R = resistance Electrical Injuries Factors Determining Severity Mucous membranes Vascular areas • volar arm, inner thigh Wet skin • Sweat • Bathtub Other skin Sole of foot Heavily calloused palm Skin Resistivity Ohms/cm2 100 300 - 10 000 1 200 - 1 500 2 500 10 000 - 40 000 100 000 - 200 000 1 000 000 - 2 000 000 Resistance of Body Tissues Least • Nerves • Blood • Mucous membranes • Muscle Intermediate • Dry skin Most • Tendon • Fat • Bone • Power lines range from: – Low: < 600 volts – Ultrahigh: > 1 million volts • Most homes in US & Canada have a 120/240 V other countries (Europe, Asia..): 220 V Immediate death may occur from: 1) Current-induced ventricular fibrillation 2) Asystole 3) Respiratory arrest secondary to: – Paralysis of the central respiratory control system – Paralysis of the respiratory muscles • Electrical current exists in 2 forms: 1) AC: (Alternating Current): when electrons flow back and forth through a conductor in a cyclic fashion • It is used in household and offices and is standardized to a frequency of 60 cycles/sec (60 Hz) 2) DC: (Direct Current): when electrons flow only in one direction • Used in certain medical equipment: defibrillators, pacemakers, electrical scalpels • AC is far more efficient and also more dangerous than DC (~ 3 times): tetanic muscle contractions that prolong the contact of victim with source Cutaneous Injuries & Burns • Extensive flash and flame burns • Hemodynamic, autonomic, cardiopulmonary, renal, metabolic and neuroendocrine responses LIGHTNING • Lightning is a form of DC • Occurs when electrical difference between a thundercloud and the ground overcomes the insulating properties of the surrounding air • Current rises to a peak in about 2 µsec • Lasts for only 1-2 sec • Voltage >1,000,000 V • Currents of >200,000 A • Transformation of the electrical energy to heat generated temperatures as high as 50,000ºF. Pathway of the current through the body: – Vertical pathway parallel to the axis of the body is the most dangerous. It involves all the vital organs; central nervous system, heart, respiratory muscles, in pregnant women the uterus and fetus – Horizontal pathway from hand to hand: the heart, respiratory muscles and spinal cord – Pathway through the lower part of the body: local damage Nervous System • Loss of conciousness, confusion & impaired recall • Peripheral motor & sensory nerves : motor & sensory deficits • Seizures, visual disturbances & deafness • Hemiplegia, quadriplegia, spinal cord injury • Transient paralysis, autonomic instability hypertension, peripheral vasospasm due to lightning from massive release of catecholamines Management of Electrical and Lightning Injuries Overall fluid management should be judicious unless: SIADH Patient Monitoring • Most severe cardiac complications present acutely • Very unlikely for a patient to develop a serious or life-threatening dysrhythmia hours or days later • Asymptomatic normal ECG do not need cardiac monitoring • Preexisting heart disease: monitor such patients for 24 hrs after the injury • Criteria for cardiac monitoring: – Exposure to high voltage – Loss of consciousness – Abnormal ECG at admission Electric Shock: What Should You Do? The victim: Felt the current pass through his/her body Yes No Was held by the source of the electric current The current passed through the heart Yes No Yes 1 second or more No Yes No Lost consciousness No Touched a voltage source of more than 1 000 volts Yes Cardiac Monitoring 24 hours Electric Shock: What Should You Do? Page 2. Touched a voltage source of more than 1 000 volts Cardiac Monitoring 24 hours Yes No Yes Has burn marks on his/her skin Yes The current passed through the heart No Evaluate and treat burns (surgical evaluation, look for myogolbinuria, etc.) No Was thrown from the source Yes Evaluate trauma No Is pregnant Yes Evaluate fetal activity No BENIGN SHOCK Reassure and discharge Direction Services de Sante Hydro Quebec, 1995 Kriteria Rujukan Pasien LB Grade 2–3 Luas LB>10% BSA pd semua umur. Umur <10 and > 50 thn Luas LB >20% BSA Mengenai area : • Face • Hand • Perineum • Eyes • Feet • Ears • Genitalia • Sendi2 utama (Major joints) 46 Kriteria Rujukan Pasien LB Grd 3 dg Luas LB> 5% BSA LB listrik, petir & Zat Kimia Trauma Inhalasi Tdp Penyakit atau trauma penyerta 47 Kriteria Rujukan Pasien LB Koordinasi dg dokter Pusat Rujukan. Dirujuk dg: • Dokumentasi/ informasi yg lengkap. • Hasil Laboratorium. 48