Febrile Neutropenia : Why empirical therapy ?
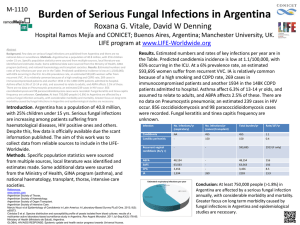
advertisement

Febrile Neutropenia revisited : what has been learnt and what remains to be learned ? Prof. Jean Klastersky, MD, PhD Institut Jules Bordet, Université Libre de Bruxelles Brussels, Belgium 1 2 The risk of infection increases with the severity and duration of neutropenia G.P. Bodey, Ann Int Med, 1966 3 Febrile Neutropenia Historical Background First description around 1900 Rare until development of chemotherapy In the 1960s: mainly in acute leukemia with profound neutropenia Gram negative sepsis common with 90 % mortality Empirical therapy with synergistic combinations of antibiotics reduced mortality to + 10 % In the1980s: development of chemotherapy for solid tumors leading to less severe and less protracted neutropenias For multiple reasons, replacement of Gram negative infections by Gram positive severity of infections decreases FN becomes a heterogeneous syndrome Risk-stratification models allow for identification of low risk patients with additional treatment options Increase of fungal sepsis in specific groups of neutropenic patients leads to widespread use of empirical antifungal agents 4 1)Prevention is essential; should the present indications for G-CSF use be extended ? 2) Empirical antimicrobial therapy remains a basic rule; can it be adapted to the risk of complications ? 3) Occult fungal infections are common in patients with prolonged neutropenia; what do we need : empirical or preemptive treatment and/or earlier diagnosis ? 5 Updated meta-analysis of prophylactic G-CSF: Infection-related mortality Disease 0.1 0.2 0.5 1 Citation Doorijian Gisselbrecht Pettengell All Lymphoma Bui Chevallier Crawford Fossa Trillet-Lenoir Timmer-Bonte Vogel All Solid Tumors Combined 2 5 Relative Risk (95% CI) 0.541 0.976 0.951 0.986 0.297 4.691 0.203 6.426 0.141 0.608 1.037 0.357 1.174 56.861 0.024 0.968 47.992 0.020 1.095 5.293 0.226 0.336 1.213 0.093 0.328 3.073 0.035 0.461 1.782 0.119 0.201 4.172 0.010 0.470 0.934 0.237 0.549 0.836 0.360 Favours G-CSF Favours No G-CSF N.M. Kuderer, JCO, 2007 6 Current Guidelines for primary prophylaxis with G-CSFs FN risk level ASCO EORTC NCCN Moderate to high (> 20 %) Use G-CSFs Use G-CSFs Use G-CSFs Intermediate (10-20 %) Recommend Consider Consider Low (< 10 %) Not specified Not recommended Not recommended ++ +++ + Consider other risk factors than intensity of chemotherapy 7 Secondary prevention of subsequent FN in patients who had a first episode CRAWFORD (1991) (n=59 SCLC) LALAMI (2001) (n=48 breast ca) Incidence of FN after the first cycle of chemotherapy (without CSF) 100% 100% Incidence of FN after the second cycle of chemotherapy (with CSF) 23% 6% 8 Outcome of FN and univariate analysis Resolution without complication : 363/416 (87%, 95% CI : 84%-90%) Resol. Compl. Death Risk of FN < 10% 180 19 (9%) 9 (4%) Risk of FN 10%-20% 123 15 (10%) 9 (6%) Risk of FN > 20% 60 11 (16%) 0 (0%) No use of prophylactic growth factors Risk of FN < 10% 167 18 8 Risk of FN 10%-20% 106 13 9 Risk of FN > 20% 48 10 0 Use of growth factors Risk of FN < 10% 13 1 1 Risk of FN 10%-20% 17 2 0 Risk of FN > 20% 12 1 0 9 Optimal schedule for G-CSF Schedules for G-CSF in breast cancer with a 7% risk of Febrile Neutropenia 480 µg/day days 8 -14 480 µg/day, days 8, 10,12,14 300 µg/day days 8 -14 300 µg/day days 8,10,12,14 *300 µg/day days 8 and 12 *equivalent to the other schedules with respect to grade 3 and 4 neutropenia P. Papaldo et al., J Clin Oncol, 2005 10 Incidence of febrile episodes, probable infections, and hospitalization for infection* Levofloxacin (N=781) Placebo (N=784) Relative Risk (95 % CI) P Value Nb of patients (%) Febrile episode Probable infection Hospitalization for infection 27 (3.5) 62 (7.9) 0.44 (0.28 – 0.68) < 0.001 109 (14.0) 152 (19.4) 0.72 (0.57-0.90) 0.005 52 (6.7) 81 (10.3) 0.64 (0.46 – 0.90) 0.01 * No effect on mortality M. Cullen et al., NEJM, 2005 11 Prophylactic levofloxacin to prevent bacterial infection in patients with hematological cancer and neutropenia Febrile Neutropenia* Placebo Levofloxacin 308/363 (85 %) 243/375 (65 %) *p = 0.001 (Mortatility and tolerability : similar) GIMEMA, NEJM, 205 12 1)Prevention (antibiotics or G-CSF’s) is essential; should the present indications be extended ? 2) Empirical therapy with broad spectrum antibiotics remains a basic rule; to be adapted to the risk of complications ! 3) Occult fungal infection should be suspected early in patients with prolonged neutropenia; do we need empirical or pre-emptive treatment ? 13 Empirical therapy with carbenicillin plus gentamicin reduced dramatically (21 %) the mortality associated with Pseudomonas sepsis Ps. aeruginosa 14 Score derived from the logistic equation of the MASCC predictive model (1386 patients with FN) Characteristic Points Burden of illness No or mild symptoms 5 Moderate symptoms 3 No hypotension 5 No chronic obstructive pulmonary disease 4 Solid tumor or no previous fungal infection in hematological ca 4 Outpatient status 3 No dehydration 3 Age < 60 years 2 Threshold: score ≥ 21(maximum 26) predicting less than 5% of severe complications J. Klastersky et al., J. Clin. Oncol. 2001 15 Medical complications considered serious Hypotension : systolic blood pressure less than 90 mmHg Respiratory failure : arterial oxygen pressure less than 60 mmHg Disseminated intravascular coagulation Confusion or altered mental state Congestive cardiac failure seen on chest x-ray and requiring treatment Bleeding severe enough to require transfusion Arrhythmia or ECG changes requiring treatment Renal failure requiring investigation and/or treatment with IV fluids, dialysis, or any other intervention J. Klastersky et al., JCO, 2000 16 Response rates and final outcome of low- and not lowrisk patients with febrile neutropenia as predicted y the MASCC risk-index score Low risk (n=58) Not low risk (n=22) Response to empiric antibiotic therapy 47 (81 %) 2 (9%) Resolution without complications 57 (98 %) 3 (14 %) 0 (0%) 8 (36 %) Death before resolution A. Uys et al., Supp. Care Cancer, 2004 p < 0.001 17 Oral Antibiotics with early hospital discharge compared with In-patient intravenous antibiotics for low-risk FN in cancer patients: a prospective randomized study Intravenous AB In patient (60) Oral AB Out patient (66) Death 1 0 Serious complications 0 1 Intolerance to AB 0 3 Persistance of fever 5 6 Mean cost per episode (£) 840 470 Mean nursing hours per episode 21 11 Innes et al., Brit. J. Cancer, 2003 18 J. Klastersky et al., JCO, 2006 19 J. Klastersky et al., JCO, 2006 20 Occurrence of serious medical complications Overall (all orally treated patients) 9/178 (5 %) Patients discharged early 0/79 (0 %) Patients not discharged early 9/99 (9 %) . patients with persisting fever 4/19 (21 %) . patients with medical reason 4/42 (9 %) . patients without medical reason 2/38 (2%) J. Klastersky et al., 2005 21 J. Klastersky et al., JCO, 2006 22 Conclusions Simplified management of FN (oral and ambulatory) has great potential for quality of life and cost reduction Our study suggests that it is feasible and safe in a significant proportion (44 %) of patients predicted to be at low risk of complications using the MASCC score Observation for 24-48 hours seems critical even if criteria for early discharge are fullfilled; 9 % of patients maintained hospitalized for « good » or « bad » reasons developed severe complications Low risk prediction and suitability for oral outpatient treatment are to some extent different issues; safe prediction of the feasibility of early discharge remains to be established. 23 Mortality in 3190 patients with febrile neutropenia 30 days after entry (IATCG trials Vb, VIII, IX and XI Bacteremia (%) No Bacteremia (%) No evaluable patients 805 2385 Causes of Death Infections Infections + other* other* 48 (5.9) 20 (205) 29 (3.6) 71 (2.9) 35 (105) 83 (3.5) P=0.001 Total n° of deaths 97 (12.0) 189 (7.9) P=0.003 (*) mainly hemorrhage and extensive cancer 24 25 Outcome and distribution : complicated versus uncomplicated bacteremias Single gram positive Single gram negative Polymicrobial Total Complications Deaths Total Complications Deaths Total Complications Deaths Clinical site of infection 128 21 % 5% 82 21 % 23 % 25 16 % 16 % No clinical site of infection 155 19 % 5% 86 24 % 13 % 23 30 % 9% J. Klastersky et al., J. Antimicrob. Chemother., 2007 26 Mortality rate in bacteremic patients stratified by classes of the MASCC score and type of bacteremia MASCC Gram+ Gramscore Total Deaths Total Deaths (Nr.) (%) (Nr.) (%) < 15 18 28 23 43 15-20 ≥ 21 89 176 6 2 64 81 23 6 Klastersky et al., J. Antimicrob. Chemother., 2007 27 Factors predicting bacteremia* (multivariate analysis) High fever (> 39°C) P < 0.001 Presence of shock P < 0.001 Clinical site of infection P = 0.04 Antifungal prophylaxis P < 0.001 Platelets > 50.000/ul P < 0.001 Duration of granylocytopenia > 6 days P < 0.001 * « when tested in the validation set, the model was poorly predictive » Adapted from Viscoli et al., Europ. J. Cancer, 1994 28 ROC curves for predicting mortality in the test population (N = 1003) AUC : MASCC : 0.778, 95% CI : 0.715-0.840 MASCC + B : 0.790, 95% CI : 0.729-0.851 MASCC + GNB : 0.791, 95% CI : 0.729-0.0.854 29 We can predict the high risk patients What can we do for improving the outcome of FN in that subset of patients ? 30 Response to empiric combination antimicrobial therapy vs monotherapy in patients with leukemia Combination(cephalosporin + Monotherapy amikacin) (cephalosporin) Klastersky et al. (1988) 6/12 1/16 Tamura et al. (2004) 33/45 24/45 39/57 (68 %) 25/61 (40 %) 31 Therapeutic CSF: Infection-Related Mortality Citation Effect Anaissie 0.320 0.032 3.184 Aviles 0.274 0.093 0.810 Biesma 3.783 Garcia-Carb 1.441 Lopez-Hern L U 0.141 101.826 0.236 8.809 0.425 0.035 5.106 Mayordomo 1.680 0.169 16.664 Ravaud 0.324 0.013 8.229 Combined 0.526 0.269 1.031 0.01 0.1 1 10 100 Favours CSF Favours No CSF 32 33 Description of patients with death within 2 weeks of Emergency Department presentation among a total of 48 admitted for neutropenic fever Age Gender Malignancy Positive ED blood cultures ICU MASCC score Description of death 55 F AML No From ED 8 Improving 2 days prior to death suddenly with cardiac arrest 35 F AML Group g strep From floor 12 Aspergillosis on lung biopsy, respiratory failure, DNR decided 58 M Waldenstrom’s No From floor 21 Bacteremia, intracranial bleed, respiratory failure, DNR decided 57 M AML No From floor 21 Was discharged recently but readmitted to palliative care, DNR decided 80 F AML Enterobacter No 19 Bacteremia, pneumonia, respiratory failure, DNR decided 93 F Myelodysplasia No No 19 DNR decided DM Courtney et al; The Oncologist, 2009 34 1)Prevention (antibiotics or G-CSF’s) is essential; should the present indications be extended ? 2) Empirical therapy with broad spectrum antibiotics remains a basic rule; be adapted to the risk of complications ! 3) Occult fungal infection should be suspected early in patients with prolonged neutropenia; do we need empirical or pre-emptive treatment ? 35 Randomized Studies Comparing Empirical Treatment with Antifungal Agents for Persisting Fever during Neutropenia YEAR STUDY ANTIFUNGAL AGENTS COMPARED 1982 Pizzo et al Conventional ampho B vs no antifungal therapy 1989 EORTC Conventional ampho B vs no antifungal therapy 1996 Viscoli et al. Conventional ampho B vs fluconazole 1998 Malik et al. Conventional ampho B vs fluconazole 1998 White et al.. Conventional ampho B vs ampho B colloidal dispersion 1999 Walsh et al. Conventional ampho B vs liposomal ampho B 2000 Winston et al. Conventional ampho B vs fluconazole 2000 Wingard et al. Liposomal ampho B vs ampho B lipid complex 2001 Boogaerts et al. Conventional ampho B vs itraconazole 2002 Walsh et al. Liposomal ampho B vs voriconazole 2004 Walsh et al. Liposomal ampho B vs caspofungin 36 FAILURES of Empirical Antifungal Therapy in Microbiologically Demonstrated Fungal Infections (FI) Liposomal ampho B (961) Breakthrough FI No cure of base line FI Total failures* *p = 0.03 Voriconazole Caspofungin (415) (556) 45 (4.6) 8 (1.9) 29 (5.2) 22 (2.2) 7 (1.6) 13 (2.3) 67 (6.9 %) 15 (3.6 %) 42 (7.7 %) J. Klastersky, NEJM, 2004 37 Prevalence of fungal infections in persistently neutropenic patients not receiving empirical therapy Pizzo et al. (1982) 18 EORTC (1989) 28* Guiot et al. (1993) 26* Corey and Boeckh (2002) 45 Maertens et al. (2005) 21 * Autopsy-based data 38 Empirical versus preemptive therapy in febrile neutropenic patients not responding patients to empirical broad spectrum antibiotic therapy Empirical vs pre-emptive approach (PE) Results Diagnosed IFI Overall survival IFI related mortality Mean cost (euros) E PE 150 patients 143 patients 4 (2.6 %) 13 (9.0 %) P < 0.02 147 (98 %) 136 (95 %) NS 0 (0 %) 3 (2.1 %) P = 0.12 3.595 3.745 NS C. Cordonnier et al., Blood, 2006 39 What do we need beyond empiric of pre-emptive therapy of suspected fungal infections in febrile neutropenic cancer patients ? 1) Predictive models of patients at risk of developing fungal infections 2) Early and specific tools for diagnosing fungal infection and monitoring therapy 3) More reliable antifungal therapies Conclusions 1) Prevention is essential : the indications for G-CSF should be extended to « low risk » patients with solid tumors 2) Empirical antimicrobial therapy : should be supplemented with more pathophysiologicallyoriented approaches and early intensive care in high risk patients 3) Occult fungal infections : require definition of high riskgroups and earlier specific diagnosis, in addition to empirical therapy The past two decades have witnessed major progress in the supportive management of cancer patients who develop fever and neutropenia. Morbidity and mortality have been dramatically reduced, and for many patients therapies are simplier, less toxic and more appropriately delineated according the patient’s risk status. Despite these progresses, however, numerous challenges remain to be addressed and important problems to be solved 42 Thank you for your kind attention and « Au revoir » 43