Neutropenia Case

RA’s Nasty Neutropenia:
To stimulate or not to stimulate
Jennifer Day
NHA Resident
March 26, 2010
Overview
Objectives
Patient Profile
Controversy
Pharmacy Intervention
Monitoring
Outcome
Objectives
Define neutropenia
List five medications that may cause neutropenia
State three patient populations where granulocytecolony stimulating factor (G-CSF) therapy would be appropriate
Reiterate the recommendations presented by the
British Columbia Centre for Disease Control
(BCCDC) for cocaine-induced neutropenia
Patient Profile – Presentation
ID: 49 yo 1 st Nations female
CC: Sore, inflamed mouth, hurt to eat
HPI : • 1 yr hx of neutropenia, recurrent mucositis
? 2 o to laced crack-cocaine
• G-CSF therapy started
• Presented to Ft. St. James (FSJ) hospital after 1 st dose w/ fever, chest pain
• Transferred to UHNBC-PG
Patient Profile – Presentation
DX:
SH:
Neutropenia non-responsive to G-CSF
PMH: Anemia, insomnia
FH: Non-contributory
Hx of EtOH abuse, gas-huffing, crack-cocaine use x ~15 years
Smoking, casual use, last use 3 weeks
Allergies: codeine = itching
Patient Profile – Medications
MPTA: G-CSF 300mcg SQ daily x 1 dose
Ibuprofen 400mg PO tid
Vitamin B6 50mg PO daily
Vitamin B12 100mg PO daily
Calcium/Vit D 500mg/125 IU PO bid
Ferrous sulphate 300mg PO bid
Oxazepam 15mg PO hs prn
Patient Profile – Medications
UHNBC: Ceftazidime 2g IV q8h
Gentamicin 360mg IV q24h
Lansoprazole 30mg PO bid
Replavite 1 tab PO daily
Folate 5mg PO daily
Ferrous sulphate 600mg PO bid
Vitamin C 1000mg PO daily
Vitamin B12 1000mcg IM qmonthly
Patient Profile – Medications
UHNBC: Nystatin 500,000 units PO tid, swish and swallow
KCl SR 24mEq PO q4h x 3 doses then
KCl SR 8mEq PO bid
Benzydamine 5mL PO qid, swish and spit
Magic Mouthwash 10mL PO prn
Hydromorphone 2mg PO q4h prn
Dimenhydrinate 25-50mg PO q4-6h prn
Patient Profile – Review of Systems
VITALS
(Oct 27)
CNS
HEENT
RESP
CVS
GI
GU
AVSS: T=37 o C, HR=75, BP=135/75, RR= 17,
SaO
2
=98% on RA
No complaints
Sore, inflamed mouth, pain with eating, white plaques; no cough/SOB
No chest pain, iron=5 ( ), iron sat = 15% ( )
Melena x 5/7, endoscopy normal; voiding per washroom, no burning/urgency/frequency (BUF)
Patient Profile – Review of Systems
LIVER
KIDNEY
ENDOCRINE
SCr=46 (stable), CrCl=151; splenomegaly;
LFT WNL
BG=5.3 (random)
MSK/EXTR/SKIN Slight facial edema, body aches
FLUID STATUS No complaints; K=2.8 ( ), Na=134 ( )
Patient Profile – Neutropenia
WBC
(x10 9 )
Hgb
(g/L)
Plts
(x10 6 )
ANC
(x10 9 )
Temp
( o C)
(FSJ)
Oct
19
0.7
115
155
--
38.9
(PG)
Oct
27
<0.5
59
34
0.1
Transfused
37
Oct
28
0.5
89
60
0.1
37 36.5
Oct
29
0.6
94
68
--
Patient Profile – Medical Problems
Neutropenia
Oral Mucositis
Oral Thrush
GI Bleed
Anemia
Pain
Hypokalemia
Pharmacy Assessment – DRPs
AR is experiencing neutropenia
AR is experiencing side-effects of G-CSF
AR is experiencing oral mucositis pain
AR is experiencing oral thrush
AR is experiencing a GI bleed
AR is experiencing hypokalemia
AR is experiencing anemia
AR is experiencing pain
Haematopoiesis – Overview
The formation of blood components from haematopoiesis stem cells found in bone marrow
–
All blood cells are of three lineages
Erythroid cells: red blood cells
–
–
Lymphoid cells: adaptive immune system
Myeloid cells: granulocytes, macrophages
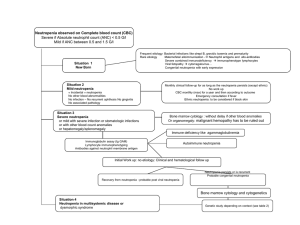
Neutropenia – Overview
Definition: ANC less than 1.5x109/L
– ANC = WBC x percent (PMNs + bands) ÷ 100
Drug-induced:
– Decreased production or peripheral destruction
Alkylating agents, antimetabolites, anticonvulsants, antipsychotics, antibiotics, anti-inflammatory agents, anti-thyroid medications, antibiotics, levamisole
Risks: mucositis, infection, sepsis
Neutropenia – Overview
ANC
(10 9 /L)
Risk Management
>1.5
None
1-1.5
No risk of significant infection; fever managed as outpt
0.5-1 Some risk of infection; fever can be managed as an outpt
<0.5
Significant risk of infection; fever should always be managed as inpt with IV ABX
<0.2
Very significant risk of infection; fever should always be managed on an inpt basis with IV ABX
Levamisole – Overview
Why lace cocaine with levamisole?
–
–
Stable under heated conditions
Increase dopamine and endogenous opiate levels
Previously used for colon cancer, rheumatoid arthritis and as an antihelmithic
– Imidazothiazole derivative ABX
Hasn’t been available commercially since 2005
–
–
Caused neutropenia by ?immune-mediated destruction
Still available in USA for veterinary use
Pharmacy Assessment – Goals
Stop disease process
Manage patient’s symptoms
Prevent disease
Normalize physiological parameters
Minimize side-effects of therapy
Neutropenia – Treatment Options
Alternatives for drug-induced neutropenia:
– 1st line:
Discontinue offending agent
Supportive care (ABX if febrile, indicated)
–
–
2nd line:
Colony-Stimulating Factor hormone
– G-CSF (Filgrastim)
– Pegylated G-CSF (Pegfilgrastim)
– GM-CSF (Sargramostim)
3rd line :
If no response to above
– IV immunoglobulin
– Granulocyte infusion
Neutropenia – Treatment Options
G-CSF
– MOA:
G-CSF is produced by monocytes
Regulates neutrophil production, progenitor differentiation
Enhances phagocytic ability
G-CSF
Neutropenia – Treatment Options
G-CSF (Filgrastim)
– Side-effects:
>10%: fever, rash, splenomegaly, bone pain, epistaxis
1-10%: hyper/hypotension, MI/arrhythmias, chest pain, headache, N/V, peritonitis
<1%: pulmonary infiltrates, tachycardia, hematuria, wheezing, renal insufficiency, injection site reaction, ARDS, allergic reactions, arthralgias, dyspnea, facial edema, hemoptysis
Controversy
G-CSF indications for patients with:
– Febrile neutropenia due to chemotherapy
– Specific chemotherapy protocols
– Bone marrow transplants
– Human Immunodeficiency Virus (HIV)
– Chronic non-drug induced neutropenia
G-CSF use in non-febrile, otherwise healthy patients is not well established
Controversy
G-CSF use for the treatment of neutropenia
– Should not be used routinely in afebrile pts
– Little supporting evidence as an adjunct to ABX therapy in febrile pts
– May be considered in high risk neutropenic febrile pts or serious infectious complications:
advanced age (older than 65 years)
fever at hospitalization or unstable fever
progressive infection or invasive fungal infections
pneumonia or sepsis syndrome
severe (ANC less than 1) or anticipated prolonged
(greater than 10 days) neutropenia
PICO Question
P: In a 49 year old First Nations woman who chronically smokes crack-cocaine and is currently experiencing afebrile neutropenia secondary to levamisole-laced cocaine
I: is G-CSF therapy versus
C: no G-CSF therapy
O: effective in decreasing mortality?
Search Strategy
Databases:
– PubMed, Embase, Google Scholar
Search terms:
– Cocaine-induced
– Levamisole
– Neutropenia
– G-CSF
Results: anger and frustration
Literature Review – Evidence
Levamisole tainted cocaine causing severe neutropenia in Alberta and British Columbia,
Harm Reduction Journal; 2009
– Retrospective, 42 cases
– 93% used crack-cocaine; 72% smoked
– Conclusions:
If fever or infection present empiric IV ABX and supportive care are recommended
“Treatment with G-CSF should be considered”
Literature Review – Evidence
Agranulocytosis associated with levamisole in cocaine, BCCDC update: April 2009
– Developed standard case report form
– Diagnostic tests: CBC & diff, urine for drugs
– Management:
If ANC <1.0, febrile with active infection: hospitalize
Infectious work-up, broad spectrum ABX
“G-CSF should not be started until consultation with haematologist”
– Recovery in 7-10 days
Literature Review – Evidence
Neutropenia during treatment of rheumatoid arthritis (RA) with levamisole, Annals of
Rheumatic Diseases, 1978
– 60 pts with RA treated with levamisole
– 35% showed persistent decrease of neutrophils
– 10% developed severe neutropenia (ANC <1.0)
– Management:
Therapy stopped
Monitored for sign of infection
Recovered within 10 days
Bottom Line
Should we use G-CSF in this pt population?
– May be considered in high risk neutropenic febrile pts or those at risk of serious infectious complications
– No evidence for decreased mortality or increased benefit over appropriate ABX for febrile neutropenia
– Consider cost vs. benefits
– BCCDC advises against routine use
– More studies and clear guidelines needed
Weighing the Options
Pros
–
–
Not contraindicated
Possibility of effect
Cons
–
–
–
No evidence
Not clearly indicated
Hasn’t worked in past
– Experiencing side-effects
– Expensive
– ? Mortality benefits
Pharmacy Recommendations
Discontinue G-CSF in this pt
– Experiencing side-effects
– No evidence, no effect
Report case to BCCDC, counsel pt on risks
Continue to monitor temperature, signs of systemic infection
Increase nystatin 500,000 units PO qid, swish and swallow
Change Magic Mouthwash 5mL PO qid ac meals
Increase benzydamine 15mL PO qid, swish and spit
Outcome
G-CSF 300 mcg SQ daily Oct 29-Nov 5
Bone marrow biopsy active
Awaiting HIV serology tests
D/C ABX, lansoprazole
Pt able to eat regular meals with minimal pain and discomfort
Oral thrush resolved
Monitoring Plan – Efficacy
Parameter
Temp < 38 o C
Frequency Who?
Twice daily Nurse, Pt CNS
HEENT
RESP
CVS
DERM
MSK
Mucositis, cough, SOB,
RR,
O
2
Sat
HR,
BP
Daily
Daily
MD, Nurse,
Pharm
Nurse
GI/GU Burning, urgency, frequency
KIDNEY SCr, urine output
Daily
HEME CBC (Neuts >1.5x10
9 /L) Daily
Nurse, Pt
Weekly/Daily MD, Pharm
MD, Pharm
Chills, night sweats, facial edema
Daily Nurse, Pt
Monitoring Plan – Toxicity
CNS
Parameter Frequency Who?
Temp < 38 o C, headache Twice daily
HEENT
RESP
CVS
Epistaxis, peritonitis, dyspnea, wheezing
Daily
HR,
BP, chest pain Daily
GI/GU Splenomegaly, N/V, hematuria
KIDNEY
LIVER
Renal insufficiency
Alk Phos
HEME CBC (WBC >10)
DERM
MSK
Rash, bone pain, injection site rxn
Daily
Weekly
Daily
Daily
Nurse, Pt
MD, Nurse,
Pharm
Nurse, Pt
Nurse, Pt,
MD
MD, Pharm
MD, Pharm
Nurse, Pt
Course in Hospital
WBC
(x10 9 )
Hgb
(g/L)
Plts
(x10 6 )
Neuts
(x10 9 )
G-CSF
Temp
( o C)
Oct
27
Oct
28
Oct
29
Oct
30
Oct
31
Nov
1
Nov
2
Nov
3
Nov
4
Nov
5
Nov
6
<0.5
0.5
0.6
0.8
0.7
0.6
0.5
0.6
0.8
1.4
1.6
59 89 94 114 113 103 105 101 99 100 102
34 60 68 102 79 86 81 96 98 87 89
0.1
0.1
-0.0
0.2
0.1
0.2
0.1
-0.5
0.6
37 36.5
37 37 36 36.5
36 36.5
38.5
38.5
37.3
Outcome
Saturday, Nov 7, 2009
– ANC = 1.2 x10 9 /L
– G-CSF dose given (18 doses total)
– Pt stable, afebrile, no signs of further infection
– Transferred back to FSJ
– Lost to follow-up
Addendum
References
Up to date
Cps
Toronto’s notes
Micromedex
Lexi drugs
Asco guidelines
Harm reduction article
Reporting form article
Questions?