a Powerpoint of this Presentation
advertisement

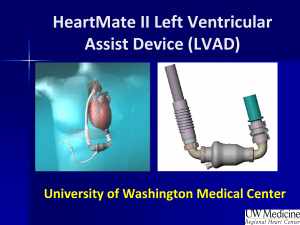
Contemporary Outcomes With the HeartMate II® LVAS David J. Farrar, PhD Vice President, Research and Scientific Affairs Thoratec Corporation J138-0711 HeartMate II® LVAS A surgically implanted, rotary continuous-flow device in parallel with the native left ventricle Left ventricle to ascending aorta Percutaneous driveline Electrically powered Batteries and line power Fixed-speed operating mode Home discharge with ability to return to activities of daily life (work, school, exercise, hobbies, etc.) Implantable Pump Percutaneous Lead Controller Batteries HeartMate II—Indications for Use HeartMate II is the first and only FDA-approved continuous-flow device for both Bridge-to-Transplantation (BTT) and Destination Therapy (DT). Bridge-to-Transplantation Risk of imminent death from nonreversible left ventricular failure Candidate for cardiac transplantation Destination Therapy NYHA Class IIIB or IV heart failure Optimal medical therapy 45 of last 60 days Not a candidate for cardiac transplantation HeartMate II—Worldwide Clinical Experience* More than 7,000 patients worldwide have now been implanted with the HeartMate II LVAS. Patients supported ≥ 1 year: 2,439 Patients supported ≥ 2 years: 851 Patients supported ≥ 3 years: 269 Patients supported ≥ 4 years: 83 Patients supported ≥ 5 years: 20 Patients supported ≥ 6 years: 1 Patients supported ≥ 7 years: 1 * Based on clinical trial and device tracking data As of March, 2011 HeartMate II—Improvement in BTT Outcomes Miller LW, Pagani FD, Russell SD, et al. NEJM. 2007;357:885-96. Pagani FD, Miller LW, Russell SD, et al. JACC. 2009;54:312-21. Starling, Naka, Boyle, et al. JACC. 2011;57:19. HeartMate II—Improvement in DT Outcomes Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361:2241-51. Park SJ. AHA Scientific Sessions, November 2010. HeartMate II—Recent Publications HeartMate II—Post-Approval BTT Study Initiated post-BTT approval to assess outcomes in a broader patient care environment First approved study to use INTERMACS The first 169 consecutive HeartMate II patients enrolled in INTERMACS Listed or likely to be listed for transplant Enrolled across 77 centers from April to August 2008 Patients followed for at least 1 year Starling, Naka, Boyle, et al. JACC. 2011;57:19. Study Endpoints Primary endpoint Survival Secondary endpoint Adverse events Reported upon occurrence Quality of life EuroQol EQ-5D visual analog scale determined at baseline and 3, 6, and 12 months postimplant Starling, Naka, Boyle, et al. JACC. 2011;57:19. Demographics and Patient Characteristics 1. Starling, Naka, Boyle, et al. JACC. 2011;57:19. 2. Pagani FD, Miller LW, Russell SD. extended mechanical circulatory support with a continuous-flow rotary left ventricular assist device. J Am Coll Cardiol. 2009;54:312-21. INTERMACS Profiles Starling, Naka, Boyle, et al. JACC. 2011;57:19. HeartMate II—Actuarial Survival Post-Approval Study Starling, Naka, Boyle, et al. JACC. 2011;57:19. HeartMate II—Adverse Events Patients in the post-approval study experienced a reduced or similar rate of adverse events in a broader patient care environment compared to clinical trial patients. There were zero pump replacements through the first 6 months of HeartMate II support in the post-approval study group. 1. Starling, Naka, Boyle, et al. JACC. 2011;57:19. 2. Pagani FD, Miller LW, Russell SD. Extended mechanical circulatory support with a continuous-flow rotary left ventricular assist device. J Am Coll Cardiol. 2009;54:312-21. Clinical Outcomes Based on INTERMACS Profile 101 BTT / DT continuous-flow LVAD patients at three centers were preoperatively categorized by INTERMACS profiles and followed to determine if there were differences in outcomes. Hypothesis that patients with higher INTERMACS profiles (lower acuity of heart failure) would have reduced lengths of stay postVAD in comparison to patients with lower INTERMACS profiles (higher acuity of heart failure). Outcomes observed included actuarial survival, survival to discharge, and length of stay. Boyle, Ascheim, Russo, et al. JHLT. 2011;30:4. Clinical Outcomes Based on INTERMACS Profile Length of Stay Post-VAD Actuarial Survival Post-VAD Less acutely ill, ambulatory patients in INTERMACS profiles 4–7 had better survival and reduced length of stay compared to patients who were more accurately ill in profiles 1–3. Group 1: INTERMACS 1 Group 2: INTERMACS 2–3 Group 3: INTERMACS 4–7 Boyle, Ascheim, Russo, et al. JHLT. 2011;30:4. Analysis of Response of Four Rotary Pumps “… the characteristic of the HeartMate II can be considered superior to the centrifugal pumps in so far that the zone of maximum preload sensitivity occurs at the low end of the afterload scale (i.e., mean afterload of 50–90 mmHg) mostly inhabited by patients requiring mechanical assistance to the left ventricle.” Salamonsen RF, Mason DG, Ayre PJ. Artif Organs. 2011. HeartMate II—Recent Presentations HeartMate II Risk Score—Study Goals Derive and then validate a risk model for predicting short- and longer-term survival following continuous flow LVAD implantation. Cowger J, Sundareswaran K, Rogers J, et al. ISHLT 2011. Lietz, et al. Circulation. 2007;116:497-505. HeartMate II Risk Score—Study Cohorts Patients undergoing HeartMate II implant enrolled into the HeartMate II Bridge-to-Transplant (N=489)1,2 and Destination Therapy (N=633)3 trials were included (total N=1,122). Patients were prospectively and randomly assigned to either the derivation cohort or to the validation cohort. Multivariable analyses were performed to identify the risk factors of death following LVAD implantation. Cowger J, Sundareswaran K, Rogers J, et al. ISHLT 2011. 1. Miller L, Pagani F, et al. N Engl J Med. 2007;357:885-96. 2. Pagani F, Miller L, et al. JACC. 2009;54:312-21. 3. Slaughter M, Milano C, Rogers J, et al. N Engl J Med. 2009;361:2241-51. Multivariate Predictors* of Death PostLVAD Cowger J, Sundareswaran K, Rogers J, et al. ISHLT 2011. Risk Stratification in HeartMate II Patients Comparison of Derivation and Validation Cohorts Cowger J, Sundareswaran K, Rogers J, et al. ISHLT 2011. Risk of Bleeding and Stroke in HeartMate II Outpatients Russell SD, Boyle A, Sun B, et al. ISHLT 2011. Preoperative Predictors of Bleeding Univariate Correlates Multivariate Risk Factors Age > 65 Albumin <=3.3 Female P = 0.003 Ischemic Etiology 0.0 0.5 1.0 1.5 2.0 2.5 Hazards Ratio Russell SD, Boyle A, Sun B, et al. ISHLT 2011. Female Gender—Only Independent Risk Factor for Stroke and Pump Thrombosis Females were twice as likely to experience a stroke or pump thrombosis event. Russell SD, Boyle A, Sun B, et al. ISHLT 2011. Impact of Infection on Stroke and Thrombosis During a ±14 day window around an infection event patients were: 4 times more likely to experience a hemorrhagic stroke event 8 times more likely to experience an ischemic stroke event 9 times more likely to experience a pump thrombosis event Russell SD, Boyle A, Sun B, et al. ISHLT 2011. Driveline Exit Site Comparison of Velour Versus Silicone Skin Interface Hypothesized that: Silicone interfaces will be associated with lower infection rates and faster incorporation times Surface characteristics will differ significantly between velour and silicone Ledford ID, Miller DV, Mason NO, et al. ISHLT 2011. Velour Versus Silicone Skin Interface Velour Silicone N=16 N=16 Mean Age (years) 55 51 Gender (M/F) 14/2 13/3 Indication (BTT/BTC/DT) 11/1/4 13/1/2 Ledford ID, Miller DV, Mason NO, et al. ISHLT 2011. Histology Velour exhibits more dermal inflammation and an irregular shaped stratum corneum. Silicone is smooth and regular, and shows less inflammation. Ledford ID, Miller DV, Mason NO, et al. ISHLT 2011. Contemporary Destination Therapy Results Park SJ. AHA Scientific Sessions, November 2010. 1. Slaughter M, Milano C, Rogers J, et al. N Engl J Med. 2009;361:2241-51 . Contemporary Destination Therapy Results The CAP results show a decrease in major adverse events. Park SJ. AHA Scientific Sessions, November 2010. Contemporary Destination Therapy Results Park SJ. AHA Scientific Sessions, November 2010. In Summary Over 7,000 patients implanted with HeartMate II—long-term durability Improvements in Bridge-to-Transplant and Destination Therapy survival and adverse event rates Adverse-event differences in LVAD patients may lead to targeted approaches for men and women Driveline infections can possibly be reduced by new tunneling techniques New HeartMate II risk model along with INTERMACS profiles may help guide future patient selection