a Powerpoint of this Presentation
advertisement

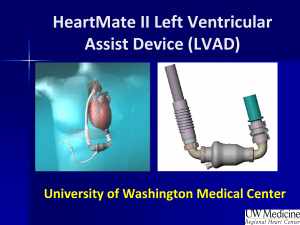
Are LVADs Ready To Be Mainstream? Joseph G. Rogers, MD Associate Professor of Medicine Duke University Medical Center J105-0311 Mainstream Therapies Address a large patient population Established safety and efficacy Have a proven track record of clinical success Have an acceptable risk / reward tradeoff Addressing An Unmet Need The VAD patient population is approaching 100,000 in the United States alone. US population1 301,000,000 Target population (35-74 age cohort)1 139,100,000 Diagnosed CHF population2 All ages 5,520,000 35-74 3,744,000 NYHA Class IIIB and IV3 in 35-74 age cohort 374,400 Comorbidities estimated in this cohort (280,800) Target VAD patient population (35-74 years) 93,600 1 US Census Bureau Statistics (2007) Heart and Stroke Statistics, American Heart Association 3 Cardiovascular Round Table research and analysis, The Advisory Board company (2009) 2 Heart Failure Has A High Mortality Rate Similar To Aggressive Malignancies Medical therapy alone can be a poor long-term treatment option for many in the more advanced stages of heart failure. Four major publications show the mortality risk associated with NYHA Class IV heart failure is high, with a 1-year mortality between 60 and 94 percent.1-4 Class IV heart failure patients treated with medical therapy alone have mortality rates similar to or greater than aggressive forms of cancer.5 1 2 Rose, Gelijns, Moskowitz, et al. NEJM. 345:1435-43, 2001. Rogers, Butler, Lansman, et al. J Am Coll Cardiol. 50:741-47, 2007. 3 Hershberger, Nauman, Walker, et al. J Card Fail. 22:616-24, 2003. 4 Gorodeski, Chu, Reese, et al. Circ Heart Fail. 2:320-24, 2009. 5 Data on file. Pleasanton, Calif: Thoratec Corp. HeartMate II®—A Proven Adjuvant Therapy For Advanced-Stage Heart Failure HeartMate II is the first and only FDA-approved continuous flow device for both Bridge-to-Transplantation (BTT) and Destination Therapy (DT). Bridge-to-Transplantation Non-reversible left heart failure Imminent risk of death Candidate for cardiac transplantation Destination Therapy NYHA Class IIIB or IV heart failure Optimal medical therapy 45 of last 60 days Not a candidate for cardiac transplantation For inpatient and outpatient use HeartMate II—Design Features Optimized blood flow Low thrombosis risk Low anticoagulation requirements Reliability - HeartMate II—Widespread Approval And Adoption Received European CE Mark in November 2005 Received FDA approval for BTT in April 2008 Received Health Canada approval in May 2009 Received FDA approval for DT in January 2010 Distributed throughout Asia and Australia European CE Mark November 2005 FDA approval for BTT April 2008 FDA approval for DT January 2010 HeartMate II—Most Widely Used, Proven Efficacious, and Durable in Broad Patient Population More than 6,000 patients, spanning over 6,000 patient years across 254 centers worldwide, have now been implanted with the HeartMate II LVAD* Patients supported 2 years: 700 Over 60 patients supported 4 or more years Longest support duration: 6 years Smallest patient: 1.1 BSA Largest patient: 3.2 BSA Age range: 11–87 *As of January 13, 2011 HeartMate II—Peer-Reviewed Publications HeartMate II has an unparalleled number of peerreviewed published studies in highly regarded publications including NEJM and JACC. Data featuring HeartMate II has been published in more than 120* peer-reviewed articles including: 3 New England Journal of Medicine 6 Journal of American College of Cardiology 5 Circulation 35 Journal of Heart and Lung Transplantation 11 Annals of Thoracic Surgery 10 Journal of Thoracic Cardiovascular Surgery *As of January 2011 Improvements With BTT Results Over Time n = 133 n = 281 n = 169 Miller, Pagani, Russell, et al. NEJM. 357:885-96, 2007. Pagani, Miller, Russell, et al. JACC. 54:312-21, 2009. Starling, Naka, Boyle, et al. JACC, in press 2010. HeartMate II—Contemporary BTT Outcomes The HeartMate II BTT post-approval study was initiated to assess outcomes in a broader patient care environment outside of a clinical setting, representing real life situations. HeartMate II Group First 169 consecutive HeartMate II patients enrolled in INTERMACS listed, or likely to be listed, for transplant 77 centers enrolled patients from April to August 2008, and were followed for at least 1 year post-implant Endpoints The primary endpoint was survival, and secondary endpoints included adverse events reported upon occurrence and functional status using the 6-minute walk test and EuroQoL scale—determined at baseline and 3, 6, and 12 months post-implant Kirklin JK, Naftel DC, Kormos RL, et al. Second INTERMACS annual report: more than 1,000 primary left ventricular assist device implants. J Heart Lung Transplant. 2010;29:1-10. HeartMate II Post-Approval Study Patient Demographics The majority of enrolled patients were noted to be INTERMACS 1 or 2. HeartMate II Post-Approval Study Actuarial Survival Operative 30-day survival was 96% and patients achieved 90% successful outcomes at 6 months and 85% at 1 year. Starling, Naka, Boyle, et al. JACC, in press 2010. HeartMate II Post-Approval Study Quality Of Life As demonstrated by the EuroQoL instrument, HeartMate II patients experienced early and sustained improvement in quality of life over the course of follow-up, with scores doubling at 12 months post-implant. Starling, Naka, Boyle, et al. JACC, in press 2010. HeartMate II Adverse Event Rates From The BTT PostApproval Study The HeartMate II postapproval study demonstrated low adverse event rates for stroke and RV failure. Stroke and RV failure rates have improved from the HeartMate II pivotal clinical trial. Events per patient year. Pagani FD, Miller LW, Russell SD. Extended mechanical circulatory support with a continuous-flow rotary left ventricular assist device. J Am Coll Cardiol. 2009;54:312-21. Starling, Naka, Boyle, et al. JACC, in press 2010. . Destination Therapy Pivotal Trial Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuous-flow left ventricular assist device. N Engl J Med. 2009;361(23):2241-51. Survival In The Destination Therapy Pivotal Trial The pivotal HeartMate II Destination Therapy trial demonstrated significant improvements in outcomes compared to randomized patients with pulsatile LVADs 68% survival at 1 year 58% survival at 2 years Slaughter MS, Rogers JG, Milano CA, et al. Advanced heart failure treated with continuousflow left ventricular assist device. N Engl J Med. 2009;361(23):2241-51. Fang JC. Rise of the machines–left ventricular assist devices as permanent therapy for advanced heart failure. N Engl J Med. 2009;361(23):2282-84. Destination Therapy Trial CAP: Overview And Baseline More than 500 additional DT patients have been enrolled under a continued access protocol (CAP). Trial Overview and Baseline Characteristics DT Trial Experience Cohort description: HeartMate II patients: Enrollment period: Early Trial Mid-Trial Primary data cohort Portion of DT CAP N = 133 N = 281 March 2005 – May 2007 May 2007 – March 2009 Mid-trial patients did not vary in baseline characteristics Park SJ. AHA Scientific Sessions, November 2010. Improvements In DT Survival Patients enrolled in the mid-trial experienced better survival. * P value adjusted for body surface area Park SJ. AHA Scientific Sessions, November 2010. DT CAP Trial Shows Significant Reductions In Adverse Events Hemorrhagic stroke > 50% reduction 0.03 events per patient year * p < 0.05 ** p < 0.01 Device-related infections > 35% reduction 0.27 events per patient year Sepsis > 25% reduction 0.27 events per patient year Park SJ. AHA Scientific Sessions, November 2010. Stroke Rates Similar To Other Cardiac Surgical Procedures HeartMate II therapy stroke rates are similar to other commonly accepted cardiac surgical procedures such as CABG and valve procedures. Incidence of stroke by cardiac surgical procedure (data collected at Johns Hopkins from 2001 – 2004) McKhann GM, Grega MA, Borowicz LM, et al. Stroke and encephalopathy after cardiac surgery - an update. Stroke. 2006;37:562-71. Boyle AJ, Russell SD, Teuteberg JJ, et al. Low thromboembolism and pump thrombosis with the HeartMate II left ventricular assist device: analysis of outpatient anti-coagulation. J Heart Lung Transplant. 2009;28:881-87. DT CAP Trial Functional Class Improvements All patients were Class IIIB or IV at baseline. n = 266 n = 191 n = 158 n = 125 n = 67 Park SJ. AHA Scientific Sessions, November 2010. DT CAP Trial Quality Of Life Improvements 343 m 74 225 m 30 Park SJ. AHA Scientific Sessions, November 2010. LVAD Survival Compared To OMM Therapy Park SJ. AHA Scientific Sessions, November 2010. Improved Timing Of Patient Referral For Evaluation A range of referral criteria assessments and scoring systems can be utilized to define the right moment to screen a patient for a HeartMate II implant.1 Appropriate timing for referral is when a patient presents in Class IIIB or IV heart failure and has more than one of the functional or laboratory risk factors. 1 Russell SD, Miller LW, Pagani FD. Advanced heart failure: a call to action. Congest Heart Fail. 2008;14:316-21. 2 Teuteberg J, Lewis E, Nohria A, et al. Characteristics of patients who die with heart failure and low ejection fraction in the new millennium. J Card Fail. 2006;12(1):47-53. Functional Assessment Inability to walk one block without shortness of breath Intolerant or refractory to ACE inhibitor, angiotensin receptor blockers, or betablockers One heart failure-related hospital admission in the past 6 months2 CRT nonresponder High diuretic dose (e.g., 120 mg/d Furosemide) Lab Assessment Serum sodium < 136 mmol/L BUN > 40 mg/dL or Serum Creatinine > 1.8 mg/dL Hemotocrit < 35% In Summary HeartMate II: Compelling data from large clinical trials demonstrates efficacy Achieved very high survival rates BTT – 90% 6 months, 85% 1 year DT – 74% 1 year, 64% 2 years Superior to what is anticipated with optimal medical management Substantial and sustained quality of life improvements Acceptable adverse event profile Case Study 67 y/o referred for advanced heart failure therapy Ischemic cardiomyopathy EF < 20% with LVEDD = 7.3 cm Cath 1 month prior: 20% pLM, 100% pLAD, stent in pLCX, 50% stenosis pOM1, 60% pRCA with diffuse 50% stenosis throughout. Patent LIMA to LAD, patent SVG to PDA with 50% proximal stenosis Thallium: anterior infarct, no ischemia ICD Co-morbidities: HTN, DM, hyperlipidemia Case Study Hospitalized once in past 6 months Progressive exertional dyspnea and fatigue (e.g., unable to climb 1 flight of stairs without dyspnea or unhappy with current level of functionality) Occasional nocturnal dyspnea No edema Appetite adequate and no weight change No ICD shocks Meds: ASA 81 mg daily, Clopidogrel 75 mg daily, Furosemide 40 mg daily, Lisinopril 10 mg daily, Metoprolol Tartrate 25 mg twice daily, Simvastatin 20 mg daily, Spironolactone 25 mg daily Case Study Examination HR=92, BP=96/78 Clear lungs Depressed carotid upstrokes, JVP=12, RRR, No S3 or murmur Trace LE edema Labs: Sodium=134mmol/L, BUN=12 mg/dl, Cr=0.8 mg/dl, BNP=436pg/ml, Albumin=3.5 g/dl Case Study Case Study Level 1 CPX Results 2 minutes and 37 seconds, Ekelund protocol Peak HR=148, Peak BP=102/71 RER=1.16 Peak VO2=11.6 ml/kg/min (49% predicted) VE-VCO2 Slope=49.8 Case Study Questions: Should this patient receive an ICD upgrade to BiV-ICD? Are there opportunities for revascularization? Are the medications optimized? Is this patient an appropriate VAD patient?