immunomodulators and biologic therapy for inflammatory
advertisement

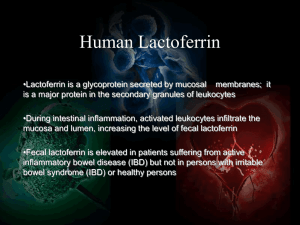
INFLAMMATORY BOWEL DISEASE IMMUNOMODULATORS AND BIOLOGIC THERAPY Inflammatory Bowel Disease (IBD) IBD ◦ Subgroups or types of IBD: Crohns Disease (CD) Ulcerative Colitis (UC) ◦ Onset across all ages reported in as young as preschoolers ◦ More commonly onset in adolescent age IBD: MULTI-FACTORIAL ETIOLOGY Environmental Trigger IBD Genetic Predisposition Immune Response Manifestations of IBD: Crohn’s Disease (CD) ◦ Extends throughout the GI tract: from mouth to anus; ◦ Commonly affects the terminal ileum & colon (terminal ileitis) ◦ Involves all layers of bowel wall (transmural) ◦ Pain characteristic to RLQ ◦ Fistula/fissure/stricture development ◦ Extra-intestinal symptoms, uveitis, large joint / arthritis, mouth ulcers, liver disease, renal calculi, cutaneous manifestations (erythema nodosum) ◦ May require surgery to manage complications ◦ Medical management, life long condition Manifestations of IBD: Ulcerative Colitis (UC) ◦ ◦ ◦ ◦ Limited to colon & rectum Involves the mucosa & submucosal layer Pain characteristic to LLQ Extraintestinal symptoms as with Crohn’s except for apthous lesions ◦ Medical management ◦ Curative surgery is a colectomy IBD: Signs and Symptoms Abdominal pain / cramps Fatigue Anorexia, weight loss and decreased growth velocity Nocturnal symptoms Systemic symptoms may be present for months or years prior to GI symptoms and diagnosis (CD) Diarrhea (bloody more common with UC) Extraintestinal involvement: joint and muscle pains, apthous oral ulcers (CD), uevitis Periods of exacerbations and remissions Sometimes differentiation between CD and UC may be difficult to determine. When differentiation is not obvious the IBD may be classified as “Indeterminate Colitis” Diagnostic Workup Abdominal series to evaluate structure and anatomy Labs: CBC, Inflammatory markers (ESR and CRP) Stool studies to rule out infectious origin Endoscopy (upper & lower may be indicated for CD) with biopsy and histiologic evaluation Serum antibody markers help to confirm diagnosis (perinuclear antineutrophil cytoplasmic antibodies [PANCA] and anti-Saccharomyces cerevisiae antibodies [ASCA]); Testing + for P–ANCA more likely to have UC while children who test + for ASCA are more likely to have Crohn’s) Nutrition as Treatment Low residue diet Nutrition is a significant first line therapy for CD ◦ (nutrition delivered by mouth, NG/G-tube or parenteral nutrition) Nutrition is a supplemental therapy for UC Vitamin and mineral supplementation (vitamin B12, folic acid, calcium, Vitamin D, iron) Pharmaceutical Treatment Aminosalicylics – anti-inflammatory; induces remission, administered topically PR Antibiotics-reduce bacterial burden in the gut Steroids-induces remission and control inflammation for maintenance therapy Immunomodulators- suppress activated inflammation; maintenance and remission Biologics-antibodies act on specific molecules in the immune cascade; maintenance and remission IBD Pharmacologic Therapies BIOLOGICS (moderate-severe disease) IMMUNMODULATORS (moderate-severe disease) ANTIBIOTICS (mild to moderate disease) STEROIDS (moderate to severe disease) AMINOSALICYLATES (mild to moderate disease) 1st three levels are mainstay of a traditional step up approach for pharmacological therapy. A combination of these agnets may be administered. This approach starts with the least toxic medical regime and advances in therapy are determined based on response. Immunomodulators and biologics are added when there has been a lack of response or side effects/ toxicities are manifested. Indications for Immunomodulators and/or Biologics Unresponsive to aminosalicyclates, steroids and antibiotics Steroid refractory/ steroid dependence Perianal disease not responding to antibiotics Fistula / stricture formation Maintenance of remission May combine therapies with lower dose steroids to achieve a “steroid sparing” effect References Crohn’s and Colitis Foundation of America. www.ccfa.org Lichtenstein, G.R., Abreu, M.T., Cohen, R., and Tremaine, W. (2006). American Gastroenterological Association Institute: American gastroenterological association institute medical position statement on corticosteroids, immunomodulators, and infliximab in inflammatory bowel disease. Gastroenterology 130 935-939. MacDermott, R.P, (2008) 6-mercaptopurine (6-MP) metabolite monitoring and TMPT testing in the treatment of inflammatory bowel disease with 6-MP or azathioprine. UpToDate retrieved 1/14/09 www.uptodate.com Prometheus® 2008. Prometheus thiopurine management. Prometheus laboratories. San Diego CA www.prometheuslabs.com Sanborn, W.J. (1996). A review or immunomodifier therapy for inflammatory bowel disease: Azathioprine, 6-mercaptoputine, cyclosporine, and methotrexate REFERENCES Snapper, S.B. and Podolsky, D.K. (2008 Immune and microbial mechanisms in the pathogenesis of inflammatory bowel disease. UptoDate retrieved 1/14/09 www.uptodate.com Su, C. & Lichtensteien, G.R. (2004). Treatment of inflammatory bowel disease with azathioprine and 6-mercaptopurine. Gastroenterology Clinics of North America 33 209-234. Taketomo, C.K. Hodding, J.H. and Kraus, Donna, M. (2008-2009). Pediatric dosage handbook. 15th edition LEXI-COMP Van Deventer, S.J. (1999). Anti-TNF antibody treatment of Crohn’s disease. Annals of Rheumatic Diseases 58 S-, 1140-1120 Wyneski, M.J., Green, A., Kay, M., Wyllie, R., Mahajan, L. (2008). Safety and efficacy of adalimumab in pediatric patients with Crohn disease. Journal of Pediatric Gastroenterology and Nutrition47(1) 19-25