Stem Cells Build New Blood Vessels to Treat Peripheral Arterial
advertisement

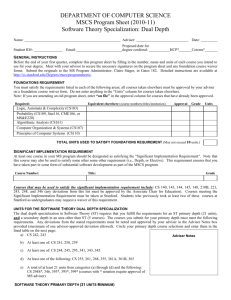
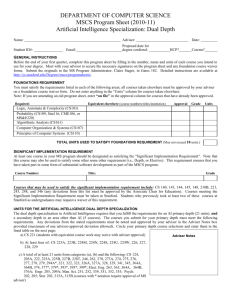
Stem Cells Build New Blood Vessels to Treat Peripheral Arterial Disease Dorota A Kedziorek, MD, Yingli Fu, PhD, Piotr Walczak, MD, PhD, Tina Ehtiati, PhD, Steffi Valdeig, Gary Huang, Jeff W.M. Bulte, PhD, Lawrence V. Hofmann, MD, Frank K. Wacker, MD, Dara L Kraitchman, VMD, PhD Johns Hopkins University School of Medicine Russell H. Morgan Department of Radiology and Radiological Science Baltimore, MD Presenter Disclosure Information I will discuss off label use and/or investigational use of contrast agents in my presentation. Financial Relationships to disclose: • Bayer Schering Pharma AG • Boston Scientific Corporation • Surgi-vision, Inc. • Siemens Healthcare USA Peripheral Arterial Disease (PAD) • PAD affects ~8-12 million Americans. • 1 in 5 patients with critical limb ischemia have severe enough disease to be ineligible for conventional medical or surgical revascularization therapy. • Normal signals to build new vessels are in foot, but problem higher in the leg. How to create new blood vessels? Problem with Current Cell Therapy Large numbers of cell are administered but fail to engraft due to: • Poor oxygen/nutrient supply • Inflammatory cytokines • Survival signals by cell-cell contact lost Zhang, Murry et al., J Mol Cell Cardiol 33, 907–921 (2001) Solution: Place Cells in “Seaweed Bubble” APA ≡Alginate-poly-L-lysine-alginate Lim and Sun, Science 1980 Biocompatible - Provides surface for cell adhesion Selective permeability - Blocks antibody and cellular destruction – good for transplanted O2, Glu donor cells VEGF, PGE2, - Permits diffusion of IL-8, IL-6, HGF, etc. nutrients and waste products. IgG, IgM Courtesy: Ming Chen Problem with Current Cell Therapy Cannot “see” where cells are injected. Needles marking injection sites What If “Imaging Visible” Capsules Were Possible? “Liquid Oxygen” •Trimodal Imaging Agent •Bromine – X-ray •Perfluorocarbon – U/S •19F - MRI C-arm CT • Flat panel detector • 16 second digital subtraction angiogram (DSA) acquisition MRI & CT of Seaweed Bubble Cells Comparison Registration Error Post-mortem/CT 2.83 ± 0.85 mm CT/MRI 0.32 ± 0.14 mm 19F MRI C-arm CT X-ray-visible & “Firefly” Stem Cells Bioluminescence Signal How to See Stem Cells in Bubble? High Low In Vivo Viability of MSCs In Vivo MSCs Viability (%) 100 Blue: Nucleus Green: Dying cell 80 60 40 20 0 0 1 3 7 Days After Administration Seaweed Plus Liquid Oxygen Plus Firefly “Brew” Seaweed (Protanal®) Liquid Oxygen (Oxygent®): _ Firefly • Happy Cells • FDA-approved agents in bubble • Better able to survive to create new blood vessels for PAD • Visible by X-ray for Interventional Radiologist to tailor therapy In Vivo Experimental Protocol Female New Zealand White Rabbits (n=21) 72 hr 2 wk Harvest SFA Occlusion • Endovascular occlusion of the superficial femoral artery with pre-occlusion angiogram ♀ ♀ Liddell et al., JVIR, 2005;16(7): 991-8. In Vivo Experimental Protocol Female New Zealand White Rabbits (n=21) XCaps + MSCs (n=5) Naked MSCs (n=5) Sham (n=6) XCaps + No MSCs (n=5) 72 hr 2 wk Harvest SFA Occlusion • Six IM injections X-ray capsules • X-ray Fluoroscopic documentation of: – X-ray Cap location – Collaterals by X-ray Angiogram XCap ♀ In Vivo Experimental Protocol Female New Zealand White Rabbits (n=21) XCaps + MSCs (n=5) Naked MSCs (n=5) Saline Sham (n=6) XCaps + No MSCs (n=5) 72 hr 2 wk Harvest SFA Occlusion XCap Histopathology Example: Empty XCap Pre-occlusion Day 14 Post-occlusion Example: Xcap with Stem Cells Pre-occlusion Day 14 Post-occlusion Efficacy of Stem Cells at Day 14 Empty Capsule XCap with Stem Cells TIMI Frame Count @ 14 Days P<0.002 P<0.01P<NS Time (sec) Time 15 10 5 0 Xcap Blank Xcaps Naked Cells N=16 Histopathology – Vessel Density CD31 Staining for Endothelium 19F and 1H MRI Trimodal Imaging c-arm CT BLI Conclusions An X-ray-visible capsule made of clinical grade components was developed that: 1. enabled targeting of injections where most needed using common interventional radiology X-ray equipment. 2. enabled determination of cell viability in vivo. 3. enhanced cell viability after administration. 4. improved therapeutic effect of creating new blood vessels for treatment of peripheral arterial disease. Acknowledgments • • • • • • • Aravind Arepally Brad Barnett Jeff Bulte Gary Huang Steffi Valdeig Ron Ouwerkerk Cliff Weiss • • • • • • • Mark Pittenger Randall Young Christine Lorenz Tina Ehtati Steve Shea Wesley Gilson Robert Krieg NIH R01-HL63439, R01-HL73223, K08 EB004348, R21-HL89029, R01-EB007825, and MD-SCRFII-0399-00