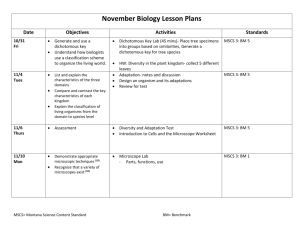
A modular approach to generating tissue engineered bone
advertisement

A Modular Approach to Generating Tissue Engineered Bone Kevin B. Miles1, Tristan Maerz2, and Howard W. T. Matthew1 1 2 Chemical Engineering & Materials Science Department, Wayne State University, Detroit, MI. Orthopaedic Research Laboratories, Beaumont Hospital, Royal Oak, MI. Modular tissue engineering involves the construction of large (macro-scale) tissue structures from smaller (micro-scale) tissue units or modules. The field has the potential to solve various cell-density related challenges associated with traditional tissue engineering. Previous studies have demonstrated the value of vascularization enhancing strategies as a necessary component in bone defect regeneration. In this study, we investigated the fabrication of macro-scale, bone-like constructs by fusion of micro-scale modular units composed of natural polyelectrolyte polymers, hydroxyapatite (HAP) granules, and mesenchymal stem cells (MSCs). The micro-scale modules were formed by complex coacervation whereby an ionic reaction between chondroitin 4-sulfate (C4S) and chitosan produced an insoluble polyelectrolyte membrane. Briefly, a C4S solution with suspended MSCs and HAP granules was extruded as 400 micron diameter droplets and collected into stirred chitosan solution. The insoluble polyelectrolyte complex was formed at the droplet-chitosan interface, encapsulating MSCs and HAP granules suspended in the C4S solution. The resulting microcapsule modules were transferred to dish culture, and maintained in a standard osteogenic culture medium. Analysis of the cultured modules over time indicated that C4S/chitosan/HAP microcapsules supported MSC proliferation and differentiation to an osteoblastic lineage. Osteoblastic activity was assessed by quantification of: bone-specific protein secretion (osteocalcin, osteopontin, collagen), calcified matrix deposition, and increases in alkaline phosphatase (ALP) activity. Moreover, the micro-scale modules could be fused post-culture to create larger (1.5 cm3) tissue constructs which possessed inherent pore spaces between the spherical, mineralized units. Fusion was accomplished by generation of additional polyelectrolyte complex between packed modules using a sequential polymer perfusion procedure. The compressive strength and elastic modulus of fused tissue constructs increased significantly during induced MSC osteogenesis, compared to values for constructs contain non-differentiating MSCs: fused constructs fabricated from microcapsules containing MSCs undergoing osteoinduction for 4 weeks exhibited a compressive strength of 6.2 MPa (+ 3.1 MPa), significantly higher than control fused constructs without differentiating MSCs (0.0059 + 0.0011 MPa). Moreover, microCT data shows that differentiating MSCs are able to extensively mineralize the walls and interior of C4S/Chitosan microcapsules: microcapsules containing MSCs osteoinduced for 4 weeks, but no initial HAP granules, exhibited a bone volume fraction of 182.5 mg HAP/cm3, compared to a bone volume fraction of zero for capsules without differentiating MSCs or HAP granules included initially in capsule fomration. Inter-module pores were found to facilitate prevascularization of constructs by culturing accessory cells, such as endothelial cells, on the exterior of the modules prior to fusion. Current studies are evaluating the effects of alternate fusion chemistries on construct mechanics and the physiology of encapsulated and accessory cells. Results to date indicate that the C4S/chitosan/HAP based module system can form the basis of either a 3D printing based or an injectable matrix based strategy for generation of vascularized bone.