Unstable Tachycardia
advertisement

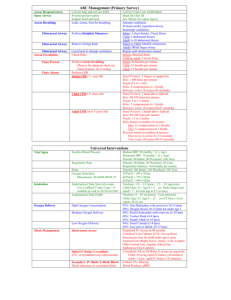
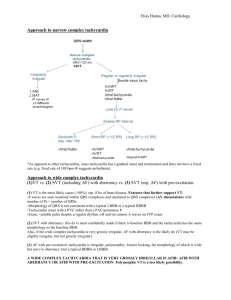
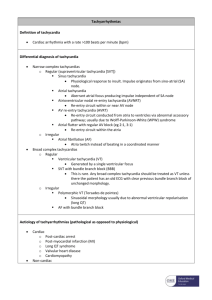
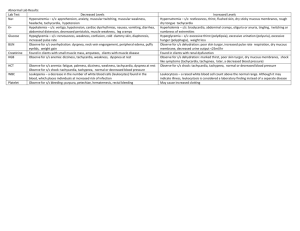
Unstable Tachycardia Hany EL-Zahaby, MD, Anesthesiologist Objectives By the end of this talk we should be able to describe or demonstrate: 1- 1ry and 2ry ABCD surveys 2- Identify unstable from stable tachycardia 3- Identify the rhythm of tachycardia 4- Determine if tachycardia is producing hemodynamic instability or the instability is producing tachycardia Objectives (cont.) 5- Follow the algorithms for tachycardia and cardioversion 6- Operation of a defibrillator/monitor to perform both defibrillation and synchronized cardioversion 7- Provide post-cardioversion care Case Scenario 52-year-old man presented to ED complaining of shortness of breath, palpitations, dizziness and severe chest pain. He is pale and sweaty. His Pulse rate is 178 and blood pressure is 81/50 Action Check responsiveness and apply primary and secondary ABCD surveys If not in cardiac arrest or VF and tachycardia is observed, order oxygenIV-monitor-fluids Identify the rhythm Supraventricular Tachycardia Atrial Flutter Atrial Fibrillation Atrial Fibrillation Ventricular Tachycardia Prepare for synchronized cardioversion Prepare oxygen saturation monitor, suction device, IV line, intubation equipment, call the code team and explain to the patient if awake Premedicate Sedatives and anesthetics: Midazolam (0.01-0.05mg/kg), Diazepam (0.05-0.1mg/kg), Ketamine(1-2 mg/kg), Etomidate (0.2-0.5 mg/kg), Thiopentone (3-5 mg/kg), Propofol (1-2 mg/kg) Analgesics: Fentanyl (1-3μg/kg) Morphine (0.05-0.1 mg/kg) Pethidine (0.5-1 mg/kg) Synchronized Cardioversion Is it equal to defibrillation? Why synchronization? When not to use synchronization? Severely unstable VT Steps for synchronized cardioversion Turn on defibrillator Attach monitor leads to the patient Ensure proper display of the patient’s rhythm (lead II) Press ‘sync’ control button Look for markers on R waves If no markers, adjust monitor gain until markers on each R Select appropriate energy level for type of arrhythmia Apply gel to paddles and position it on patient (sternum and apex) Announce to team-members “Charging defibrillators-stand clear” Press charge button on apex paddle (right hand) When the defibrillator is charged state firmly: “I am going to shock on three. One, I am clear. Two, you are clear. Three, everybody is clear” Apply 25 Ib pressure on both paddles Press the “discharge” buttons simultaneously Check the monitor, if tachycardia persists, increase the joules according to the algorithm Reset to “sync” mode after each synchronized cardioversion If VF occurs, switch to “defibrillation” mode and follow the VF/Pulseless VT algorithm Energy levels: Standard sequence is 100 J→ 200 J → 300 J → 360 J Exceptions: Atrial flutter 50 J→ 100 J→ 200 J→ 300 J→ 360 J Polymorphic VT 200 J→ 300 J → 360 J Post-conversion care: Closely monitor vital signs Continue oxygen-IV-monitor-fluids Search for a cause for this tachycardia and treat it If VF occurs, recognize need to defibrillate Documentation Conclusion Always start with ABCD Unstable means either patient or tachycardia Unstable tachycardia is treated with synchronized cardioversion Steps for cardioversion should be strictly followed THANK YOU