tachycardia patients
advertisement

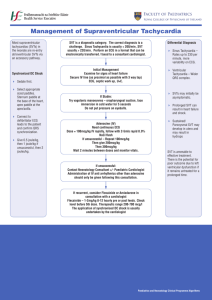
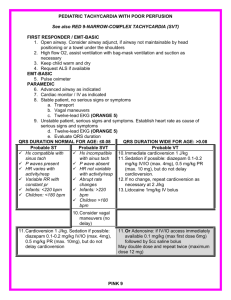
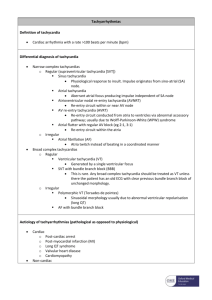
2.2.3 Cardiac Arrhythmias Author: Rob Birkinshaw Background : Dysrhythmias are common in the A&E department. Some patients tolerate them well and others become acutely unwell due to a poor cardiac output. It is important to differentiate those that need emergent treatment from those in whom treatment can be delayed until expert advice is sought. Call for senior help early , particularly if your patient is hypotensive or has chest pain. Key Points Always assess the patient first. Treat the patient and NOT the monitor. A patient who is talking is usually tolerating their rhythm. Perform simple manoeuvres first (give oxygen, get an IV line and perform vagal interventions if you suspect SVT) Analyse the ECG methodically. Get a SENIOR early if your patient is compromised. Do not try to treat it yourself. Bradycardia Note: Sinus bradycardia may be physiological in hypothermia or in very fit athletes 1.Heart block Management depends on the underlying cause. a)Acute myocardial infarction Inferiors:- heart block rarely needs to be treated with an inferior AMI. Complete heart block may be symptomatic and should initially be treated with Atropine and then by transcutaneous pacing. Anterior:- temporary pacing is indicated for complete heart block with anterior AMI as this is associated with ventricular standstill. Again initial management should be with Atropine and / or temporary pacing but always transfer the patient with the external pacer available. b)Chronic conduction diseases Complete heart block and high grade second degree block usually require permanent pacing. Atropine and transcutaneous pacing can be used as a temporising manoeuvre Syncopal patients should be treated as soon as possible which in A & E means transcutaneous pacing. Bradycardia treatment algorithm link is below: http://www.resus.org.uk/pages/bradpost.pdf Broad complex tachycardia: This may be due to Ventricular Tachycardia or a Supraventricular Tachycardia with aberrant conduction (which is quite rare). VT is characterised by AV dissociation, concordance, capture and fusions beats on the 12 lead ECG. It is a malignant rhythm usually occurring in patients with coexisting ischaemic heart disease and there is usually systemic upset secondary to a poor cardiac output. SVT can be tolerated much better unless the rate is such that myocardial perfusion is impaired. Adenosine can be used to distinguish SVT with aberrant conduction from VT if the patient is stable in many cases. Always treat the patient not the monitor; if in doubt it’s safer to treat as VT. Key points Get senior help early Use the ALS guidelines for the management of Broad Complex Tachycardias Patients with signs of cardiovascular compromise require cardioversion Check Potassium on the blood gas analyser Supraventricular Arrhythmias Supraventricular tachycardias a. Sinus tachycardia is usually not of abrupt in onset and has a rate of <150, always check for underlying problem, eg hypoxia, pyrexia etc. Treatment is that of the underlying cause. b. Paroxysmal atrial tachycardia (SVT) is usually abrupt in onset and rate >150. These patients may have chest pain and be hypotensive if the rate impairs myocardial perfusion. The rate may be slowed by vagal manoeuvres eg valsalva against a closed glottis or CSM, always check for a bruit before trying this. If the patient is compromised then cardiovert with a DC shock starting at 70 -100J. The best drug to use for chemical cardioversion is adenosine, start with 6mg iv, wait 2 min then repeat with 12mg, followed by 12 mg. Don't forget to warn the patient that they may experience a heavy feeling in the arms and chest pain. If adenosine doesn't work then it probably isn't a SVT! c. Atrial flutter The atrium always flutters at 300 bpm, the ventricles can't respond to this and there is always an element of block, so suspect it in rates that are approx 150 bpm(2:1 block). Again if the patient is compromised then DC cardiovert. d. Atrial fibrillation. This is very common affecting >10% in the over 70s. It may be a response to an underlying illness such as pneumonia, sepsis, neoplasm or ischaemic heart disease. It is important to ascertain how long the rhythm has been established for as this influences treatment. The decision is whether the patient requires rate control with digoxin or cardioversion chemically with amiodarone. At present this depends on individual clinical judgement. Guidelines are being developed to help in this process. As usual if the patient is hypotensive and unwell they should be considered for cardioversion. Acute cardioversion whether chemical or electrical carries a risk phenomenon particularly if AF has been established for at least 48 hrs. of embolic How to digitalise someone....0.5 mg of digoxin in 100 ml of normal saline over 30 mins, this can be repeated every 6 hrs to a total dose of 1.5-2.0 mg. Try and get a potassium before digitalisation, a low K potentates digoxin induced arrhythmias. Key points Correct biochemical abnormality If there is serious cardiovascular compromise then cardiovert Use the ALS guidelines for the management of Narrow Complex tachycardias Tachycardia treatment algorithm link is below: http://www.resus.org.uk/pages/tachpost.pdf