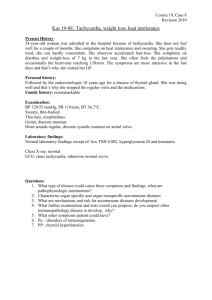
Tachycardia/tachyarrhythmia is defined as a rhythm with a HR > 100 bpm. An unstable tachycardia exists when CO is reduced to the point of causing serious S&S’s. - Serious S&S’s: cp, signs of shock, SOB, AMS, weakness, fatigue, and syncope. One important question you may want to ask is: “Are the symptoms being caused by the tachycardia?” If the symptoms are being caused by the tachycardia tx the tachycardia. Causes: There are many causes of both stable and unstable tachycardia and appropriate tx within the ACLS framework requires identification of causative factors. - Before initiating invasive interventions, reversible causes should be identified and tx. The most common causes of tachycardia that should be treated outside of the ACLS tachycardia algorithm are dehydration, hypoxia, fever, and sepsis. There may be other contributing causes and a review of the H’s and T’s of ACLS should take place as needed. Administration of OXYGEN and NORMAL SALINE are of primary importance for the tx of causative factors of sinus tachycardia and should be considered prior to ACLS intervention. 1 *Once these causative factors have been ruled out or treated, invasive tx using the ACLS tachycardia algorithm should be implemented. Associated Rhythms There are several rhythms that are frequently associated with stable and unstable tachycardia: Supraventricular tachycardia (SVT) Atrial fibrillation Atrial flutter Monomorphic VT Polymorphic VT Wide-complex tachycardia of uncertain type The first question that should be asked when initiating the ACLS tachycardia algorithm is: “Is the patient stable or unstable?” The answer to this question will determine which path of the tachycardia algorithm is executed. Unstable Tachycardia Patients with unstable tachycardia should be treated immediately with synchronized cardioversion. If a pulseless tachycardia is present patients should be treated using the cardiac arrest algorithm. The initial recommended synchronized cardioversion voltage doses are as follows: Narrow Regular: 50-100 J, i.e., SVT and atrial flutter Narrow Irregular: 120-200 J biphasic or 200 J monophasic, i.e., atrial fibrillation Wide Regular: 100 J, i.e., monomorphic VT Wide Irregular: defibrillation dose (not synchronized) Stable Tachycardia Pt’s with stable tachycardia are treated based upon whether they have a narrow or wide QRS complex. The following flow diagram shows the treatment regimen for stable tachycardia with narrow and wide QRS complex. Stable (narrow QRS complex) → vagal maneuvers → adenosine (if regular) → betablocker/calcium channel blocker → get an expert Stable (wide/regular/monomorphic) → adenosine → consider antiarrhythmic infusion → get an expert 2