background transfusion of rbc units fy2011
advertisement
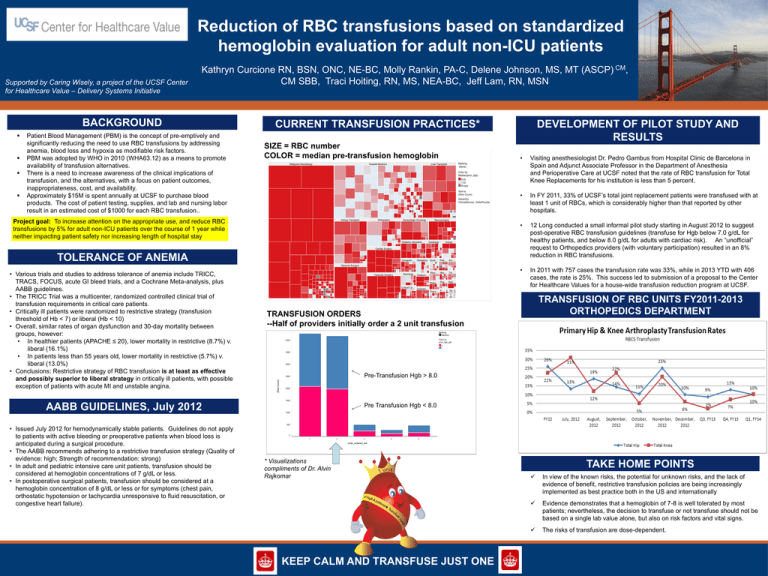
Reduction of RBC transfusions based on standardized hemoglobin evaluation for adult non-ICU patients Supported by Caring Wisely, a project of the UCSF Center for Healthcare Value – Delivery Systems Initiative Kathryn Curcione RN, BSN, ONC, NE-BC, Molly Rankin, PA-C, Delene Johnson, MS, MT CM SBB, Traci Hoiting, RN, MS, NEA-BC, Jeff Lam, RN, MSN BACKGROUND Patient Blood Management (PBM) is the concept of pre-emptively and significantly reducing the need to use RBC transfusions by addressing anemia, blood loss and hypoxia as modifiable risk factors. PBM was adopted by WHO in 2010 (WHA63.12) as a means to promote availability of transfusion alternatives. There is a need to increase awareness of the clinical implications of transfusion, and the alternatives, with a focus on patient outcomes, inappropriateness, cost, and availability. Approximately $15M is spent annually at UCSF to purchase blood products. The cost of patient testing, supplies, and lab and nursing labor result in an estimated cost of $1000 for each RBC transfusion.. CURRENT TRANSFUSION PRACTICES* SIZE Page (2)= RBC number Transfusion Orders by Service and Attending COLOR = median pre-transfusion hemoglobin Transfusions without indication of "active bleeding" Malignant Hematology Hospital Medicine DEVELOPMENT OF PILOT STUDY AND RESULTS • Visiting anesthesiologist Dr. Pedro Gambus from Hospital Clinic de Barcelona in Spain and Adjunct Associate Professor in the Department of Anesthesia and Perioperative Care at UCSF noted that the rate of RBC transfusion for Total Knee Replacements for his institution is less than 5 percent. • In FY 2011, 33% of UCSF’s total joint replacement patients were transfused with at least 1 unit of RBCs, which is considerably higher than that reported by other hospitals. • 12 Long conducted a small informal pilot study starting in August 2012 to suggest post-operative RBC transfusion guidelines (transfuse for Hgb below 7.0 g/dL for healthy patients, and below 8.0 g/dL for adults with cardiac risk). An “unofficial” request to Orthopedics providers (with voluntary participation) resulted in an 8% reduction in RBC transfusions. • In 2011 with 757 cases the transfusion rate was 33%, while in 2013 YTD with 406 cases, the rate is 25%. This success led to submission of a proposal to the Center for Healthcare Values for a house-wide transfusion reduction program at UCSF. Marking: (None) Liver Transplant Color by Median(prior_hgb) 8.00 7.00 Empty Size by (Row Count) Hierarchy ClinicalService, OrderProvide Project goal: To increase attention on the appropriate use, and reduce RBC transfusions by 5% for adult non-ICU patients over the course of 1 year while neither impacting patient safety nor increasing length of hospital stay Kidney Transplant Orthopedics Gynecologic Oncology Pediatric Hematolo … Neurosurgery Cardiology Urology Cardiac Surgery TOLERANCE OF ANEMIA Congestiv … Obstetrics Gyne … Pedi … Em … General Surgery Vascular Surgery Neurology Neur … Hep … Tra … Otolaryn… Pedia … Plas … Rad … Critical Ca … Colorect … Thora … P … C Pe O C Int A P P P TRANSFUSION OF RBC UNITS FY2011-2013 ORTHOPEDICS DEPARTMENT TRANSFUSION ORDERS Page --Half of providers initially order a 2 unit transfusion Number of Units Ordered Red segment indicates a transfusion threshold below 8 g/dL and blue a threshold above 8 g/dL Marking: Marking Color by prior_hgb_gt8 4000 0 1 3500 3000 Pre-Transfusion Hgb > 8.0 2500 (Row Count) • Various trials and studies to address tolerance of anemia include TRICC, TRACS, FOCUS, acute GI bleed trials, and a Cochrane Meta-analysis, plus AABB guidelines. • The TRICC Trial was a multicenter, randomized controlled clinical trial of transfusion requirements in critical care patients. • Critically ill patients were randomized to restrictive strategy (transfusion threshold of Hb < 7) or liberal (Hb < 10) • Overall, similar rates of organ dysfunction and 30-day mortality between groups, however: • In healthier patients (APACHE ≤ 20), lower mortality in restrictive (8.7%) v. liberal (16.1%) • In patients less than 55 years old, lower mortality in restrictive (5.7%) v. liberal (13.0%) • Conclusions: Restrictive strategy of RBC transfusion is at least as effective and possibly superior to liberal strategy in critically ill patients, with possible exception of patients with acute MI and unstable angina. CM (ASCP) , 2000 1500 AABB GUIDELINES, July 2012 • Issued July 2012 for hemodynamically stable patients. Guidelines do not apply to patients with active bleeding or preoperative patients when blood loss is anticipated during a surgical procedure. • The AABB recommends adhering to a restrictive transfusion strategy (Quality of evidence: high; Strength of recommendation: strong) • In adult and pediatric intensive care unit patients, transfusion should be considered at hemoglobin concentrations of 7 g/dL or less. • In postoperative surgical patients, transfusion should be considered at a hemoglobin concentration of 8 g/dL or less or for symptoms (chest pain, orthostatic hypotension or tachycardia unresponsive to fluid resuscitation, or congestive heart failure). Pre Transfusion Hgb < 8.0 1000 500 0 1 2 3 4 5 units_ordered_le4 * Visualizations compliments of Dr. Alvin Rajkomar KEEP CALM AND TRANSFUSE JUST ONE TAKE HOME POINTS In view of the known risks, the potential for unknown risks, and the lack of evidence of benefit, restrictive transfusion policies are being increasingly implemented as best practice both in the US and internationally Evidence demonstrates that a hemoglobin of 7-8 is well tolerated by most patients; nevertheless, the decision to transfuse or not transfuse should not be based on a single lab value alone, but also on risk factors and vital signs. The risks of transfusion are dose-dependent.