Blood products - Vula
advertisement

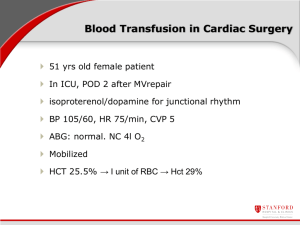
Blood Products in Critically ill Children Shamiel Salie Paediatric Intensive Care Unit Red Cross Children’s Hospital, University of Cape Town 1818 - Extracted 4 ounces of blood from the arm of the patient’s husband with a syringe and successfully transfused it Anaemia in critically ill children • Causes – Chronic anaemia – Overt and occult blood loss – Bone marrow suppression from diseases/treatment – Inadequate erythropoietin response to anaemia Red Blood Cell Transfusions • For decades considered to be a low risk with obvious benefits • 10/30 rule • Restrictive use of blood since the 1980’s What actually happens in PICU? • 50% of children in PICU’s transfused Bateman: Am J Resp Crit Care Med 2008 • Large variability in clinical practise • Bedside observational studies Gauvin 2000 & Armano 2005 – transfusion threshold ranges from 7 - 11 g/dl • 30 North American PICU’s – Pretransfusion Hb 9.7 g/dl Bateman: Am J Resp Crit Care Med 2008 Physiological benefits of RBC transfusions • Tissue hypoxia may be due to low Hb concentration, cardiac output or SaO2 • Oxygen delivery exceeds requirements • Adaptive processes as oxygen delivery decreases with anaemia – Increased oxygen extraction – Increased heart rate and stroke volume – Preferential perfusion of head and heart at the expense of splanchnic perfusion • Altered physiological adaptation to low Hb in critically ill children – Increased metabolic rate in SIRS increases oxygen consumption and lowers reserves – Impaired LV function and vascular tone restricts oxygen delivery and blood redistribution – Infants have high resting heart rates, which limits the ability to increase cardiac output Microcirculatory effects of transfused RBC • Global increase in oxygen delivery with potentially decreased microcirculatory flow – Increased blood viscousity – Cytokines my cause vasoconstriction – Low levels of 2,3 DPG shifts curve left, impeding oxygen availability – Decreased RBC membrane deformability – Free Hb may bind NO causing vasoconstriction Immunologic effects of RBC transfusion • Some evidence that it may cause – Immune suppression by altering lymphocyte reactivity – Pro inflammatory: cytokines in unfiltered rbc’s might trigger SIRS or multi organ failure When should critically ill children be transfused? • 637 critically ill children • Equivalence of restrictive strategy (Hb<7) and liberal strategy (Hb <9.5) • No difference in MODS, death, icu stay and sepsis • 44% reduction in blood transfusions • 50% of study children transfused • • • • • 838 critically ill adults Restrictive strategy (Hb<7) and liberal strategy (Hb <9) Restrictive group had 54% fewer rbc units Decrease mortality in adults who were less sick Possible exceptions: unstable angina and MI’s • 1269 Kenyan children hospitalized for malaria English, Lancet 2002 – RBC transfusion decreased mortality in severe anaemia, <4g/dl or if Hb < 5g/dl and dyspnoeic - some benefits to keep Hb > 5 in hospitalized children • Haemodynamically unstable children: Hb > 10 • De Oliveira et al (Intens. Care Med. 2008) – children with severe sepsis – significant reduction in 28 day mortality (11% vs 39%, p=0.002) and new organ failure – targeting SVC sats > 70% using fluids, inotropes and blood transfusions keeping Hb > 10g/dl • Similar outcomes in adults using goal directed therapy Rivers et al, NEJM 2001 • Children with severe congenital heart disease and traumatic brain injuries might need higher Hb’s Transfusion related acute lung injury (TRALI) • Aetiology poorly understood • Diagnostic criteria – Acute lung injury occurring within 6 hours of a transfusion – No signs of fluid overload – Bilateral lung infiltrates on cxr • Usually resolves within 48 hours Leukocyte reduced RBC’s • Reduces leukocytes by up to 99% • reduces the number of cell associated viruses: cmv, herpes and ebv • May reduce transmission of prions and parasites and incidence of TRALI Fresh Frozen Plasma • Treatment of DIC and replacement of clotting factor • Effectiveness judged by cessation of bleeding. • aPTT and INR poor predictor of bleeding Gajic: Crit Care Med 206 • Not recommended as a volume expander Platelets • Thrombocytopenia and qualitative platelet defects impairs ability to form platelet plugs • Risk of massive bleeding when platelet count < 10 and IVH when platelets <1 • No scientific basis for keeping platelets > 20 Cryoprecipitate • Rapid increase in fibrinogen levels in patients with DIC and active bleeding • Meta-analyses of 24 studies, 1419 patients • 6% increase in mortality or ‘1 death for every 17 patients given albumen’ • Meta-analysis of 55 trials, 3504 patients • No difference in mortality • Nearly 7000 patients • No significant difference in mortality • Similar rates of secondary outcomes – Survival time, organ dysfunction, duration of mechanical ventilation, length of icu and hospital stay • Albumin to saline ratio 1: 1.4 Conclusions • Stable critically ill children can support an Hb > 7 • Maintain Hb > 10 in haemodynamically unstable children, those with significant cardiovascular disease and traumatic brain injuries Conclusions • Advantages to using leukocyte reduced blood • Platelet transfusion thresholds not evidence based • Prophylactic use of FFP is controversial Questions