Transfusion - Mississippi Valley Regional Blood Center
advertisement

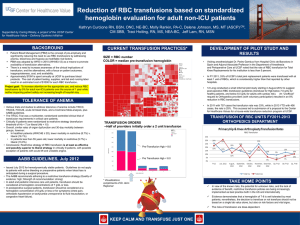
MVRBC Technical Advisory Committee: Jan. 17, 2012 Louis M. Katz MD Louis M. Katz MD Mississippi Valley Regional Blood Center Davenport, IA EVP, Medical Affairs Mississippi Valley Regional Blood Center Adj. clinical professor, IM/ID, UIHC Carver College of Medicine Premise(s) of blood management “Blood still kills” Blood still costs money, and transfusion costs much more Growing evidence supports much more restrictive transfusion strategies than used in most venues Why are restrictive triggers appropriate? primum non nocere SHOTs woefully under-reported Description of putative “new” serious hazards Pro-inflammatory Immunosuppressive Large prospective trials (TRICC, TRIPICU, PINT, FOCUS, TRACS) demonstrate outcomes at least as good using restrictive triggers Positive impact of liberal triggers on functional outcomes not demonstrated in (FOCUS) Activity costs of transfusion Residual risk from RBC transfusion Carson et al. Submitted. 2012 Global Red Cell Utilization Rates: 2008-09 RBCs per 1,000 Population 60 50 40 30 20 10 0 Source: D Devine et al.: International Forum/Inventory Management Vox Sanguinis 2009 TRICC: Primum non nocere? Restrictive (7 gm) Liberal (10 gm) Mortality Length of stay n=418 % n=420 % p 30 day 78 18.7 98 23.3 .11 60 day 95 22.7 111 26.5 .23 Hospital 93 22.2 118 28.1 .05 ICU 11.010.7 11.5 11.3 .53 Hospital 34.8 19.5 35.5 19.4 .58 “A restrictive strategy of red-cell transfusion is at least as effective as and possibly superior to a liberal strategy in critically ill patients.” NEJM. 1999. FOCUS results Units transfused Liberal trigger (n=1007) Restrictive trigger (n=1009) 1866 652 (97% transfused) (41.5% transfused) Median units 2 (IQ 1-2) 0 (IQ 0-1) 1 outcome 35.2% 34.7% 60 day mortality 7.6% 6.6% In-hosp ACS, death 4.3% 5.2% Readmit, fall, fatigue, function Carson et a.l. NEJM. 2011 No differences Costs of surgical RBC transfusion $522 Austria Activity-based cost $154 RBC acquisition cost $611 Switzerland $194 $726 Rhode Island $203 $1,183 New Jersey $248 $0 $200 Shander et al. Transfusion. 2010. $400 $600 $800 $1,000 $1,200 Getting the ground ready Admin and doc buy-in (oh, and trust) Center Hospital Clinical people who know their way around medical documentation at the facilities Access and IT resources Simple (reproducible) data requirements What we have done Initial pitch(es) to admin and medical in support of conservative transfusion Confidentiality in writing IT preparation to find the records we need Record review Data analysis and reporting Multiple presentations of the data Process development to the level they allow Reaudit (just starting) MVRBC RBC trigger audits • Descriptive manual chart audit of RBC units given. Generally during a single quarter • Record ordering physician and specialty • Hemoglobin on admission, at time of 1st order (i.e. “transfusion trigger”) and after transfusion • Documentation of bleeding in medical record • DRG, ICD-9 • Hypothesis generating Number of units ordered for 1st transfusion 3000 2500 16 audits at 14 hospitals (or systems) 2000 1500 1000 500 0 0 1 2 3 4 6 Units 8 10 Hgb in nonbleeding patients during episode of care 16 14 12 10.6 10.5 Grams 10 9.1 8 8.3 TRICC 6 4 Admission 1st transfusion Post-1st DC Hemoglobins associated with perioperative transfusions 20 18 16 14 12 12.1 Grams 10 8 10.6 10.4 8.4 FOCUS 6 4 Admission 1st transfusion After 1st DC Hbg trigger with no bleeding: by hospital 14 12 10 Grams 8 8.2 8.3 8.1 8.1 7.7 7.7 8.5 8.4 8.1 8.6 8.8 8.5 7.9 8.4 7.6 7.9 TRICC 6 4 2 1 2 3 4 5 6 7 8 9 10 10A 11 12 13 14 9A Hbg trigger for perioperative transfusion: by hospital 14 12 10 9.1 8.8 8.4 Grams 8 8.7 8.3 8.6 8.1 8.4 8.1 8.5 8.7 8.0 8.0 FOCUS 7.6 6 4 2 1 2 3 5 6 7 8 9 10 10A 11 12 14 9A Caveat emptor Reliable as our ability to find info in the record Confounders (e.g. cardio-respiratory compromise, severity of illness) not sought (TRICC says don’t matter) Acuity of intra-operative bleeding hard to assess DRG/ICD-9 numbers too small for real analysis Denominators can be hard to get, especially for inter-hospital comparisons Retrospective, manual audits AIM-II software: “concurrent”, automated audits AIM-II software Conclusions Transfusion in acute hemorrhage best left to judgment at the bedside consensus guidelines 91% of non-bleeders transfused above TRICC 76% with operative bleeding transfused above FOCUS Attention to non-bleeding & periop patients with an emphasis on EBM will reduce RBC use Discharge hemoglobin levels suggest that an emphasis on single unit transfusions will be useful Reduction = direct $$ and clinical savings Barriers Lack of basic training in transfusion medicine at all levels “This is how Dr. Osler taught me to do it…” “My patients are sicker…” “I’ve never seen TRALI…” Resources for real-time decision support and intervention Process IT support (including AIM-II?) Clinical (“real docs”) champions Barriers Hospital-acquired infections Falls Med errors Readmissions etc., etc.… ad nauseum. This is about getting on the priority menu for resources (people and time) (TJC was supposed to fix this)