Blood Transfusion Issues - NI School Final FRCA
advertisement
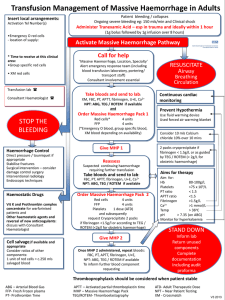
Final FRCA Study Day Blood Transfusion Issues Mary P. Mc Nicholl Haemovigilance Practitioner 25th October 2013 Overview How to respond in a timely & appropriate manner when a patient has a massive haemorrhage. ABO incompatible transfusions. Transfusion Reactions. Background - MHP Oct 2006 to Sep 2010 - 11 deaths & 83 incidents - patient harm relating to delays in provision of blood in acute situation (NPSA). RRR issued by NPSA 21.10.10. Approved by DHSSPS 18.11.10 - Circular Reference: HSC (SQSD) 16/10. WHSCT Major Haemorrhage Protocol (MHP) active since May 2011. Key Points Local protocols with a trigger phrase. Dedicated communicator with Blood Bank & Support Services (ie Porters). Early / easy release of blood components from Blood Bank. All cases reviewed by Hospital Transfusion Committee & delays/problems investigated locally / reported externally as required. DEFINITION OF MAJOR BLOOD LOSS Loss of one blood volume within a 24hr period – Normal adult blood volume approx 70ml/kg ideal body weight; 80-90ml/kg in children. Loss of 50% blood volume within 3 hours. Loss of blood at rate in excess of 150mls/minute. Correction of low haemoglobin Immediately – uncrossmatched group O negative Group Specific – 15 minutes after accurately labelled sample delivered to Blood Bank Crossmatched – 45 minutes after accurately labelled sample delivered to Blood Bank Uncrossmatched Group O Negative blood available in Altnagelvin – Satellite Blood Fridge, Recovery Area, Theatres Communication of Emergency Clinical area must ensure Blood Bank aware of patient with haemorrhage ASAP. Locally agreed & well understood trigger term:‘I want to activate the Major Haemorrhage Protocol’ Provide the following information: 1. Patient details. 2. Clinical situation. 3. Clinical area. 4. Urgency of Blood Components. 5. What Blood Components to be sent to Clinical Area. 6. Contact details (Name & Contact Number) of person nominated to be responsible for liaising with Blood Bank. Use term ‘In relation to Activation of Major Haemorrhage Protocol in A&E …’ for all subsequent calls to Blood Bank. 2nd Phone Call when activating MHP - - Contact Porters. State ‘I have activated the Major Haemorrhage Protocol.’ Inform Porter: Clinical Area Where to go (eg to Satellite Blood Fridge for uncrossmatched O negative blood; to clinical area to collect sample; to Blood Bank to collect units). Porter will remain between Clinical Area & Blood Bank until the MHP is deactivated. Blood Bank Protocol on Activation BMS will prepare:– 6 units red cells (45 minutes from receipt of sample) – 4 units Fresh Frozen Plasma (takes 30 minutes to thaw) – Order 2 units Platelets from NIBTS, Belfast Group specific blood (available 15 minutes after accurately labelled sample sent to Blood Bank) – safer than emergency O negative. 213830 213830 Stand Down At the point where emergency is perceived to be ended contact Blood Bank. State ‘I want to deactivate the Major Haemorrhage Protocol.’ Blood Bank will then make contact with Porters. Key Learning Points Need for positive patient identification. Need for accurately labelled samples. Excellent communication required between Clinical Area/Blood Bank/Porters. Know the WHSCT Major Haemorrhage Protocol… Emergency Transfusions BBT3 states: Every effort must be made to monitor vital signs during emergency transfusions. A list of all blood components / blood products transfused during the emergency should be recorded. Uncrossmatched O negative units have no patient details. Prior to administering units: - Confirm units are O Rh D negative. - Check expiry date and pack for leaks/ clumping. If uncrossmatched O negative unit used, remove this label & stick in the patient casenotes under current admission notes. Please ensure that accurate patient identification details are completed on the Blood Traceability Record as well as details, time & date that staff members remove, receive & administer the unit & then return to Blood Bank. ABO incompatible transfusions SHOT 2012 Transfusions in UK remains very safe (2.9 million components issued in 2012, very few deaths*). However, errors continue to put patients’ lives at risk, particularly from ABO incompatible transfusions. 13 ABO incompatible transfusions. 4 transfusions resulted in major morbidity (“Never Event”). *Risk of death: 1 in 322, 580 components issued; Risk of major morbidity 1 in 21,413 components issued. Risk of transfusion-transmitted infection much lower. DoH ‘Never Events’ list 2011/12 New addition – Death or serious harm as a result of the inadvertent transfusion of ABO-incompatible blood components Transfusion Reactions Transfusion Reactions Most common is an Acute Transfusion Reaction (allergic, severe febrile or anaphylactic). Acute Transfusion Reactions & TransfusionAssociated Circulatory Overload (TACO) carries highest risk for morbidity & death. SHOT 2012 – 43% of reported cases of TACO resulted in death or major morbidity. TACO Transfusion Associated Circulatory Overload Any 4 of the following that occur within 6 hours of a transfusion:- Acute respiratory distress - Tachycardia - Increased blood pressure - Acute or worsening pulmonary oedema - Evidence of positive fluid balance (BCSH, 2012) Remember Importance of correct completion of all steps in the transfusion process, particularly the final check at the bedside, & not making assumptions about the safety of the steps prior to this (SHOT, 2012). Advice & Enquiries Haemovigilance Practitioners, Altnagelvin Hospital 02871345171 Ext 213794 / 213793 Or Bleep 8434 Or Contact Blood Bank EXT 213830