BIDMC VAP Prevention Initiative - Cardiothoracic Surgery Residents
advertisement

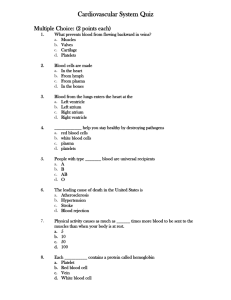
Blood Transfusion in Cardiac Surgery 51 yrs old female patient In ICU, POD 2 after MVrepair isoproterenol/dopamine for junctional rhythm BP 105/60, HR 75/min, CVP 5 ABG: normal. NC 4l O2 Mobilized HCT 25.5% → I unit of RBC → Hct 29% What is the problem? Blood transfusions are….. Inherently dangerous Each transfusion poses new set of immune challenges: increase in serious complications, ICU and hospital length of stay, as well as short term and long term mortality rates. Transfusions are not risk free and cause some degree of harm in every patient. Serious morbidity and mortality increase with the amount transfused. By some estimates each unit of allogeneic blood increases nosocomial infection rates by 50%. Risks of Blood Transfusion Fatal hemolytic reaction (1:500,000) HIV (1:7,800,000), HCV (1:1,935,000), HBV (1:220,000) Other infections (CMV, Yersinia, malaria, West Nile) Human herpesvirus-8 (NEJM 2006; 355:1331) Immunomodulation (anti-leucocyte antibodies) → TRALI (priming: recent surgery, active infection) Perioperative infection Cancer Problem of “old blood”: decreased deformability, 2,3DPG, pH and NO. Transfusion and Perioperative Infection Hill, J Trauma 2003; 54:908 Meta-analysis of 20 perioperative studies Increased odds ratio (OR = 3.45) for postoperative bacterial infection Transfusion and Cardiac Surgery Gerber, Crit Care Med 2008; 36:1068 Blood Transfusion in the ICU Hébert, N Engl J Med 1999; 340:409 −838 ICU patients with Hgb < 9 within 72 hours of admission −Randomized to transfusion Hgb trigger of 7 or 10 (restrictive vs. liberal) Trial Results (I) All results favored the restrictive (Hgb 7) strategy Trial Results (II) Subgroup analyses Decreased 30 day mortality in less severely ill patients (9% vs. 16%) Decreased 30 day mortality in patients < 55 years (6% vs. 13%) Equal mortality in patients with cardiac disease (21% vs. 23%) Risks and Benefits of Transfusion Marik, Crit Care Med 2008; 36:2667 Systematic review of 45 observational trials −1 study demonstrated benefit > risk −2 studies demonstrated benefits = risks −42 studies with risks > benefits −Pooled OR for death 1.7 (1.4 – 1.9) −Pooled OR for infection 1.8 (1.5 – 2.2) −Pooled OR for ARDS 2.5 (1.6 – 3.3) Blood usage Comparison (For all Blood products transfused) FY09 Blood Usage Comparison (includes RBCs, Platelets, Plasma) Units per Discharge Units per Discharge 3.00 2.82 2.50 2.00 1.79 1.50 1.71 1.64 1.54 1.46 1.43 1.35 1.31 1.27 1.00 1.21 1.16 0.98 0.50 - Source: UHC 2009 Blood Management Special Project Hospital - Number of Units of Blood Transfused Compared to its peers, SHC utilizes more than twice the units of blood per discharge. isoCABG PostOp RBC Usage Total Pts 2006 n=126 2007 n=90 2008 n=91 2009 n=102 60 50 40 30 20 10 0 2006 2007 2008 2009 RBC Used % Mean Units Median Units (of all pts) (pts w RBC's) (pts w RBC's) 57.9 46.7 42.8 43.1 3.4 2.3 3.4 * 4.5 ^ * 1 pt w 35 units – mean 2.6 w/o outlier ^ 1 pt w 50 units – mean 3.4 w/o outlier 2 2 2 2 AVR only PostOp RBC Usage 80 60 Total Pts 2006 n = 30 2007 n = 47 2008 n = 68 2009 n=101 40 20 0 2006 2007 2008 2009 RBC Used % Mean Units Median Units (of all pts) (pts w RBC's) (pts w RBC's) 56.7 59.6 55.9 62.4 5.2 3.6 2.9 3.8 4 2 2 3 Comparison of SHC 4+ RBC Unit Use with STS Like Group Iso AVR Iso CABG 20 40 15 30 10 20 5 10 0 4+ RBC IntraOp% 4+ RBC PostOp% 2006 14.3 19.0 2007 11.1 2008 0 4+ RBC IntraOp% 4+ RBC PostOp% 2006 30.0 36.7 8.9 2007 19.1 17.0 4.4 8.8 2008 19.1 20.6 STS Like 2008 11.9 10.2 STS Like 2008 11.8 12.7 2009 8.8 8.8 2009 16.8 23.8 Stanford Blood Transfusion Management Guidelines Proposal MULTI MODALITY APPROACH BA Reitz PJA van der Starre Stanford Blood Transfusion Management Guidelines Proposal Bleeding Risk Assessed Preoperatively − Age and weight − Hct and Platelet count − Anti-platelet therapies Stop clopidogrel 5 days pre op Continue ASA for low risk, stop 2 days for high Stanford Blood Transfusion Management Guidelines Intra-Operative Management − Cell saver and Cell salvage − Anti-fibrinolytic drugs for high risk − DDAVP for high risk only − Retrograde priming − Autologous hemodilution − R-FVIIa for recalcitrant bleeding only − Topical hemostatics Blood Transfusion Algorithms Proposal Transfusion indicated Hgb ≤ 6.0 on CPB Hgb ≤ 8.0 in high risk (age > 65, and/or co-morbidity). Acute blood loss (30% of blood volume). Rapid blood loss without immediate control. Hgb ≤ 10 g/dl in certain patients with critical end-organ ischemia. Ferraris VA, et al. STS Guidelines on blood conservation. Ann Thorac Surg, 2007. Transfusion not indicated Hgb ≥ 10 after CPB without critical end-organ ischemia. Uncertain benefit of transfusion Hgb between 8 -10g/dl in a stable patient benefit is unclear. Stanford Blood Transfusion Management Guidelines Proposal Minimize blood draws Erythropoietin Iron and nutrition Non Heme blood products used only as indicated for bleeding, with point of care testing (TEG!) Endorsement Clinical practice guidelines for the transfusion of red blood cells and platelets endorsed throughout Medical Staff leadership Medical Executive Committee Department Chairs, Kevin Tabb, Bryan Bohman Blood Transfusion Taskforce Norm Rizk, Dan Arber, Tim Goodnough, Clarence Braddock, Magali Fontain, Lisa Shieh, Maurene Viele, Paul Maggio, Ron Pearl, Pieter van der Starre Clinical Effectiveness Leadership Team John Norton, Neil Olcott, Ann Weinacker, Joe Hopkins, Pravene Nath Evidence-based Guidelines RBC Guidelines (for Hemo-dynamically stable, non-bleeding pts): Transfusions indicated only for pts with Hgb <7g/dl (for post-cardiac surgery pts and pts with acute coronary syndrome Hgb <8 g/dl ). Platelet Guidelines A single dose of platelets (adult: one apheresis product) is generally recommended as it increases the platelet count by 30,000- 60,000/ µL. (Guidelines for transfusions are based on specific disease states with corresponding platelet count triggers) EPIC Interventions: Tools to help adherence to guidelines Platelet Order template in EPIC (Live in Sep 2010) Embedded into the Blood product Order screen: Decision support built in to check the previous Platelet level prior to ordering additional units. Guidelines on disease states/platelet levels that trigger the requirement of platelet transfusion. Indications for platelet transfusion needs to be identified when ordering Best Practice Alert (BPA) for RBC Transfusions Pulls in most recent hemoglobin values and scans diagnoses on the problem list for active bleeding If the requested transfusion does NOT meet the guidelines, a “pop up” reminder flashes EPIC Best Practice Alert (BPA) : Live July 2010 Platelet Guidelines A Single Dose of platelets (adult: one apheresis product) generally recommended as it increases the platelet count by 30,000- 60,000/ µl Single unit of platelets indicated Platelet count ≤ 10,000/ µL Platelet count ≤ 20,000/ µL and signs of hemorrhagic diathesis Platelet count ≤ 50,000/ µL in a patient with active hemorrhage Platelet count ≤ 50,000/ µL in a patient with invasive procedure (recent, in-progress, planned) Platelet count ≤ 100,000/ µL in a patient with bleeding in a closed anatomical space (eg. CNS) Platelet dysfunction with active or anticipated hemorrhage (TEG?) Platelets in Epic Where do we stand now? Despite the development of RBC guidelines and the Epic BPA, the vast majority of RBC transfusions (60%) continue to occur at a Hgb of 8 or above Increased guideline adherence will Decrease clinical complications resulting from transfusion Preserve a precious resource Reduce overall blood utilization What you need to do!! Follow the RBC and Platelet guidelines developed by the Blood Task Committee and endorsed by the Medical Staff leadership BPA will remind you For actively bleeding patients, document appropriate diagnosis in the in the problem list. Transfuse a single unit of platelets Indicate the rationale for ordering platelets while placing the order. Communicate this expectation to your peers and to your house staff Incorporate the blood guidelines, and the clinical reasoning behind them, into the teaching and communication provided to interns and residents Direct feedback or questions to Blood Task Force regarding adoption of guidelines