Haemopoiesis and anaemia - PBL-J-2015
advertisement

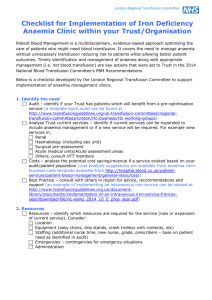
Haemopoiesis and anaemia Outline the process of haemopoiesis identifying the major cell types Haemopoiesis refers to the formation of blood, especially its formed elements, in haemopoietic tissue. From infancy onwards, the red bone marrow begins to produce all seven kinds of formed elements. All formed elements of blood trace their origins to a common type of bone marrow stem cell called the pluropotent stem cell (PPSC). The three main types of haemopoiesis is RBC, WBC and Platelet formation. RBC production is called erythropoiesis and occurs in the myeloid tissue (bone marrow).. PPSCErthyrocyte colony forming unit (receives receptor for hormone erythrop[rotein that stimulates this pathway) Erythroblast (Hb is formed here)reticulocyte (nucleus is discharged and reticulocytes enters blood circulation)Erythrocyte (mature RBC in blood) WBC production is called Leukopoiesis and occurs in Lymphoid (liver, spleen and thymustissue. This also begins with the PPSC in the bone marrow but the majority do not stay there but migrate and continue their development in other lymphoid tissues. The PPSC then differentiate into three distinct types of CFUs that go on to produce precursor cells for a variety of WBC’s: 1. Myeloblastsgranulocytesneutrophils + eosinophils +basophils 2. Monoblasts monocytes 3.Lymphoblasts B & T Cells and natural killer cells. Platelet production is called thrombopoiesis. PPSCmegakaryoblasts (form by binding to hormone thrombopoietin) many mature in bone marrow but some migrate to lungs and produce platelets there. List the major causes and types of anaemia and describe the roles of haematinic agents, decreased erythrocyte production and haemolysis in its classification. Anaemia is defined as a qualitative or quantitative deficiency of hemoglobin found inside (RBCs). Normal ranges are 130-170g/L (males) & 120-150g/L (females). Since hemoglobin normally carries oxygen from the lungs to the tissues, anaemia leads to hypoxia (lack of oxygen). The three main categories of anemia include: 1. Hemorhagic anemia due to excessive blood loss – acute hemorrhage, or chronic: Referred to as Microcytic and Hypochromic anaemia, can be a result of: Trauma, hemophilia, menstruation, ruptured aneurysm, ulcer. 1. Ineffective haemopoiesis due to inadequate erythropoiesis/Hb synthesis (Megaloblastic) Occurs when RBC DNA synthesis and subsequent cell division is impaired due a number of possible causes; lack of folate, vitamin B12 or iron (dietary related) , deficiency in EPO secretion (renal insufficiency) or intrinsic factor (pernicious), destruction of heaemopoietic tissue (hypoplastic and aplastic) . 2. Reduced RBC levels: excessive blood cell destruction – haemolysis Can be due to; congenital defects (sickle cell disease or thalassemia), drud reactions (penicillin allergy), or immune-mediated disease (hemolytic disease of the newborn), parasitic infection (malaria) , transfusion reactions. In this case RBC morphology is usually normal, but the cell count is low (normocytic-normochromic anaemia). Relate standard haematology reports to types of anaemia Full blood count parameters include: Packed Cell Volume (PCV): the proportion of the total blood volume taken by RBC: 0.4-0.5 Mean Cell Volume (MCV): the average volume of each REC: 80-100 femolitres (fL) Mean Cell Haemoglobin (MCH): av haemoglobin content of a RBC : 27-34 picograms (pg) Mean Cell Haemoglobin Concentration (MCHC): average haemoglobin concentration in a volume of packed RBC: 310-360 g/L. Conditions for Microcytic / hypochromic MCV < 80 fL MCH < 27 pg Anameia types: Iron deficiency, Thalassemia Conditions for Normocytic / normochromic MCV: normal MCH: normal Anaemia types: Haemolytic anaemia Conditions for Macrocytic MCV > 100 fL Anaemia types: megaloblastic anaemia Haematinic agents are chemicals which improves the quality of blood by increasing the Hb content by way of stimulating RBC production. Examples include iron, liver extract and Bvitamins.