Infections of the Brain Parenchyma
advertisement

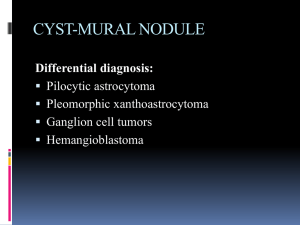
Infections of the Brain Parenchyma Cerebral Abscess Localized area of suppurative inflammation in the brain • The cavity contains thick pus formed from necrotic, liquefied brain tissue and large numbers of neutrophils and is surrounded by a fibrogliotic wall. Etiology • Large variety of bacteria; • Anaerobic bacteria (bacteroides) and anaerobic streptococci are common. • Staphylococcus aureus,& gram-negative enteric bacteria • Cerebral abscesses occur as complications of other diseases Pathology • Grossly, a cerebral abscess appears as a mass lesion in the brain. • liquefied center filled with pus and a fibrogliotic wall whose thickness depends on the duration of the abscess • The surrounding brain tissue frequently shows vasogenic edema Clinical Features & Diagnosis • (1) Features of a space-occupying lesion, including evidence of increased intracranial pressure (headache, vomiting, papilledema) and focal neurologic signs, • (2) Features relating to the source of infection, such as chronic otitis media, suppurative lung disease, and endocarditis; and • (3) General evidence of infection, such as fever, (elevated ESR), and weight loss in chronic cases. • In untreated cases, the abscess progressively enlarges and may cause death from increased intracranial pressure or rupture into the ventricular system • (CT) scan or (MRI). • Lumbar puncture is dangerous because of the risk of precipitating tonsillar herniation. • The CSF may be normal or may show mild increases in protein, neutrophils, and lymphocytes • CSF cultures may or may not be positive. Treatment • Surgical evacuation of the abscess • Antibiotic therapy is effective treatment and has reduced the previously high mortality rate of cerebral abscess to about 5–10%. Viral Encephalitis • the etiologic virus is identified in only about 30% of cases. • Worldwide, many cases of acute cerebral dysfunction in which no attempt is made to identify a virus probably go unreported. Pathology • The virus usually reaches the brain via the bloodstream. • It infects brain cells, • Causing neuronal necrosis and marked cerebral edema => leads to acute cerebral dysfunction => increased intracranial pressure. • Perivascular lymphocytic infiltration characteristic • Hemorrhages in severe Clinical Features • Acute onset with fever, headache, and signs of brain dysfunction, • Convulsions may occur. • There may be papilledema • In many cases of viral encephalitis, there is concomitant meningeal inflammation • Lumbar puncture with examination and culture of CSF may provide an etiologic diagnosis. Treatment • Therapy is supportive. • Control of cerebral edema with high doses of • The mortality rate from severe viral encephalitis is high, • and patients who recover are frequently left with permanent neurologic deficits due to irreversible neuronal necrosis Poliomyelitis • • • • Poliovirus, (enterovirus) Fecal–oral route. Through the intestine Infects the brain and spinal cord via the bloodstream. • Routine immunization during childhood The poliovirus selectively infects • (1) The meninges, producing acute lymphocytic meningitis • (2) The lower motor neurons in the anterior horn of the spinal cord and medulla oblongata. • Loss of motor neurons causes acute paralysis of affected muscles. • typically asymmetric and flaccid, with muscle atrophy and loss of deep tendon reflexes. • With time, the atrophic muscles may undergo fibrous contracture. Rabies • Rare in humans but occurs in a variety of wild animals and domestic pets(dogs and cats), • Fatal illness called hydrophobia characterized by abnormal behavior, difficulty in swallowing, and convulsions. • Humans are infected when bitten by an infected animal. • The rabies virus enters the cutaneous nerve radicles at the site of inoculation • And passes proximally to the central nervous system. • The incubation period is 1–3 months and is shortest in facial bites. • Severe necrotizing encephalitis that maximally affects the basal ganglia, hippocampus, and brain stem. • Infected neurons show diagnostic eosinophilic intracytoplasmic inclusion bodies (Negri bodies). • Electron microscopy and immunoperoxidase techniques. • fever and generalized convulsions that are precipitated by the slightest of sensory stimulations such as a gust of wind, a faint noise, or the sight of water. • Death is inevitable. • • • • • Because there is no treatment, Prevention is essential and Consists of controlling the disease in wild animals, Rabies immunization of domestic pets, and Administration of antirabies vaccine to humans immediately after viral exposure Parasitic Infections Toxoplasmosis • Toxoplasma gondii is a protozoal parasite • definitive cycle in the intestine of cats. • Humans become infected through contact with cat feces containing infective forms of the parasite. • Cerebral toxoplasmosis occurs in two distinct forms, congenital and acquired. Congenital Toxoplasmosis • Fetal infection with T gondii occurs transplacentally in the third trimester of pregnancy. • Infects the fetal brain and the retina, leading to extensive necrosis, calcification, and gliosis. • Many infants die soon after birth • those who survive have a variety of defects such as microcephaly, hydrocephalus, mental retardation, and visual disturbances. Acquired Toxoplasmosis • Rarely causes cerebral lesions in normal individuals. • Opportunistic infection in aids • Cerebral toxoplasmosis in AIDS is characterized by the presence of multiple necrotic lesions ranging in size from 0.5 to 3 cm. • Toxoplasma pseudocysts and tachyzoites may be seen in biopsies of lesions. • Diagnosis in tissues is aided by staining for Toxoplasma antigens by immunoperoxidase techniques • (1) Cerebral malaria, due to Plasmodium falciparum. • (2) African trypanosomiasis (sleeping sickness). This is caused by Trypanosoma rhodesiense in East Africa and Trypanosoma gambiense in West Africa. • (3) Cysticercosis, due to the larval form of Taenia solium, the pork tapeworm. • (4) Hydatid cyst, due to the larval form of Echinococcus granulosus. • (5) Trichinosis, due to Trichinella spiralis. • (6) Schistosomiasis, due to Schistosoma haematobium and Schistosoma mansoni (in the Middle East). • (7) Amebiasis, due to Entamoeba histolytica, which causes brain abscesses. Free-living amebae of the genera Acanthamoeba and Naegleria are rare causes of meningoencephalitis.