Virtual Reality Gaming for Treadmill Training: Improving Functional
advertisement
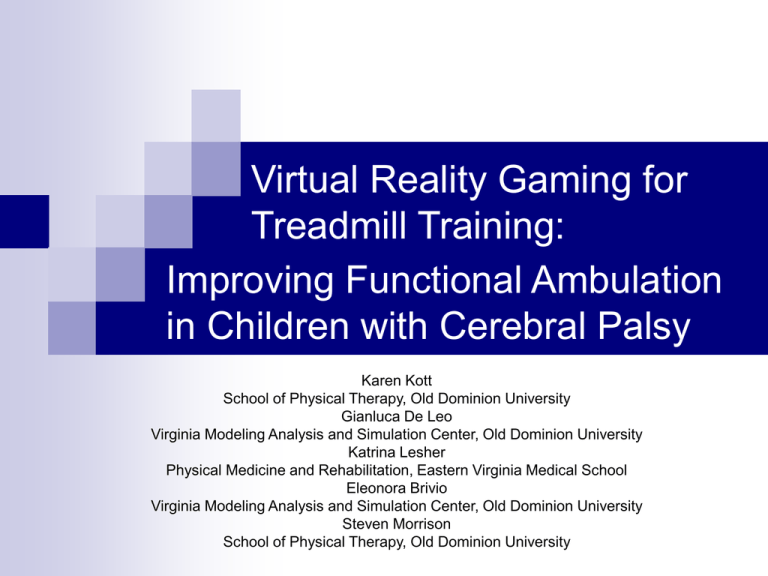
Virtual Reality Gaming for Treadmill Training: Improving Functional Ambulation in Children with Cerebral Palsy Karen Kott School of Physical Therapy, Old Dominion University Gianluca De Leo Virginia Modeling Analysis and Simulation Center, Old Dominion University Katrina Lesher Physical Medicine and Rehabilitation, Eastern Virginia Medical School Eleonora Brivio Virginia Modeling Analysis and Simulation Center, Old Dominion University Steven Morrison School of Physical Therapy, Old Dominion University Background Cerebral Palsy1 Describes group of permanent disorders that are non-progressive (2-3/1,000) Occur in the fetal or infant brain Impact development of movement and posture Causing activity limitation Background Different clinical presentations Abnormal muscle tone (hypertonia & hypotonia) Abnormal coordination (ataxia) Movement abnormality (dystonia & athetosis) Accompanying impairments Sensation, perception, cognition, communication, behavior, seizures Secondary musculoskeletal system i.e. weakness and limited range of motion Background Functional mobility or activity limitation Means to classify severity of movement disability Key function of ambulation Ambulation is the basis for standardized system of classification Gross Motor Function Classification System (GMFCS)2 Loss or limited ambulation Impacts the lifetime costs for care3 Limits the quality of life Can lead to an early death4 Literature Review Rehabilitation Ambulation training “Best practices” for motor learning movements5 Self-initiated and useful Able to adapt to the environment Practiced repetitively Goal driven related to functional tasks Treadmill feasible tool for CP6 How to make it interesting? Integrate with play and Virtual Reality (VR)7,8 VR + gait training can change spatiotemporal parameters9 Research Pilot Study Purpose: Design, develop, and test the use of a virtual game to improve ambulation in children Participants: CP ages 5-15 years ability to walk with no assistive devices except orthoses no cardiopulmonary limitations Research Study Methods: One group: pre-test/post-test design Measurement tool: Standardized Walking Obstacle Course (SWOC)10 Research Study Treatment Protocol Watch VR DVD (5,10,15 minutes segments) Walk on treadmill (completing 9 hours of training) Initial speed calculated from walk hands free condition of the SWOC Monitor HR via pulse Increased speed as tolerated by .1 mph Safety and rest Receive reinforcement via coins, diamonds and verbal prompting VR Game Solution Toys do not have rules or goals Puzzles have goals Games have rules and goals A game must include Play activity Pretended reality A nontrivial goal Rules VR Game Solution 1) design of the virtual environments, 2) render of the virtual environments, 3) edit of the final video. Lightwave application software Rendered on a cluster Solution available on DVD VR Game Solution Positive reinforcements by: Receiving verbal feedbacks from VR characters (“keep walking we have to save the princess”) Earning points. Points accumulated in the concrete form of diamonds, coins, magic shield, staff and glue (used to fight the dragon at the end) that adhered to a magic shirt that the child wore. The use of the magic shirt helped the child feel more immersed in the game. VR Game Solution QuickTime™ and a Sorenson Video 3 decompressor are needed to see this picture. Results 35 60 30 50 20 15 40 35 40 Time in Seconds 25 Time in Seconds Time in Seconds Average (SD) time all children pre-test to post-test condition of: 30 20 10 10 30 25 20 15 10 5 5 0 0 1 0 Pre and Post Tests walk with hands free 2 Pre and Post Tests walk with tray 1 2 Pre and Post Tests walk with glasses Results -) Positive feedback from subjects, their brothers and sisters and their parents -) All of the subjects completed the training (ca. 9 hours of walking) References 1.Bax, M., Goldstein, M., Rosenbaum, P., Leviton, A., Paneth, N (2007) Proposed definition and classification of Cerebral Palsy. Developmental Medicine & Child Neurology, 109, 49: 571-576. 2. Palisano, R.J., Hanna, S.E., Rosenbaum, P.E., Russell, D.J., Walter, S.D., Wood, E.P, Raina, P.S., Galuppi, B.E. (1997). Development and reliability of a system to classify gross motor function of children with cerebral palsy. Developmental Medicine & Child Neurology, 39, 214-223. 3. Economic Costs Associated with Mental Retardation, Cerebral Palsy, Hearing Loss, and Vision Impairment --- United States, 2003 Morbidity and Mortality Weekly Report (2004), 53, 03, Jan 30. 4. Day, S.M., Wu Y.W., Strauss, D.J., Shavelle, R.M., Reynolds, R.J. (2007) Change in ambulatory ability of adolescents and young adults with cerebral palsy. Developmental Medicine & Child Neurology, 49, 647-653. References 5. Valvano, J. (2005). Neuromuscular systems: the plan of care. In S. Effgen (Ed), Meeting the physical therapy needs of children. Philadelphia: FA Davis. 258-266. 6. Richards, C.L., Malouin, F., Dumas, F., Marcoux, S., Lepage, C.,Menier, C. (1997). Early and intensive treadmill locomotor training for young children with cerebral palsy: a feasibility study. Pediatric Physical Therapy, 9,4, 158165. 7. Rodgers, S., Ziviani, J. (1999) Play based occupational therapy. International Journal of Developmental Disability Education, 46, 337-365. 8. Grealy, M.A., & Heffernan, D. (2000). The rehabilitation of brain injured children: the case for including physical exercise and virtual reality. Pediatric Rehabilitation, 4, 2, 41-9. 9. Deutsch, J.E., Merians, A.S., Adamovich, S., Poizner, H.,Burdea, G.C. (2004). Development and application of virtual reality technology to improve hand use and gait of individuals post-stroke. Restorative Neurology and Neuroscience, 22, 3-5, 371-86. References 10. Held, S.L., Kott, K.M.,Young, B. (2006). Standardized Walking Obstacle Course (SWOC): reliability and validity of a functional measurement tool in children who are developing typically and atypically. Pediatric Physical Therapy, 18, 1, 23-30.