Changes in Peripheral Nervous System
advertisement

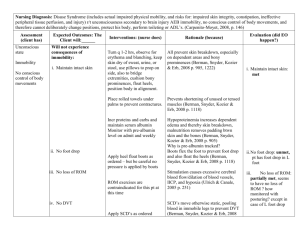
Neurosensory: Altered Cerebral Function and Increased intracranial pressure (IICP) Marnie Quick, RN, MSN, CNRN Etilogy/Patho Altered Cerebral Function: Consciousness Dynamic state in that it fluctuates Continuum from awareness of self and environment to unawareness Consciousness to deep coma Caused by: lesions/injury to the reticular system or cerebral cortex Metabolic disorders Altered Cerebral Function: Arousal/cognition (LOC) Patho/assessment Reticular Activating System (RAS) meshwork of gray cell within brainstem/thalamus. Controls wakefulness, arousal and alertness. Cerebral cortex outer layer of gray cell bodies of brain. Controls cognition, thought process. Reticular Activating System (RAS) Altered Cerebral Function: Assessment of arousal/cognition (LOC) Observe individual’s behavior, call name Verbal response to person/place/time/event If unable- how responds to commands If unable- how responds to central pain stimuli Assessment of arousal/cognition (Respiratory and pupillary light reflex) Respiratory- changes occur as brainstem is being compressed Pupillary light reflexSensory: CN 2 Motor: 3 Note pupil size; darken room; shine light in and note reaction and size Direct/consensual Assessment Arosual/cognition (EOM’S) Eye movement- CN 3,4,6 In COMA- test EOM’s Oculocephalic reflex Doll’s eyes- Sensory- CN 8; Motor- CN 3,4,6 Good Dolls eyes: eyes move in opposite direction of head movement Bad/negative Dolls eyes: eyes do not move head turned Assessment arousal/cognition (Motor) Strength, symmetry and ability to move Order from best to worse: Purposeful Generalized response Posturing- flexion or extension Flaccid Planter Reflex- Babinski testing Meningeal signs- Brudzinski, nuchal rigidity Decorticate posturing- abnormal flexion Decerebrate posturing- abnormal extension Planter Reflex and Babinski testing Common manifestations/Complications Coma states and brain death Irreversible coma- persistent vegetative state Locked-in Syndrome (not true coma) Does not have functioning cerebral cortex Caused by anoxia or severe brain injury Sleep-wake cycles; chew/swallow/cough, no track Functioning RAS/cortex; pons level interference Aware, communicate with eyes Brain death Loss of all brain function- flat EEG, no blood flow Prognosis of individual with altered cerebral functioning Outcome varies according to underlying cause and pathologic process The longer the individual unconscious, the longer has absent Doll’s eyes; the poorer the cognitive recovery Residual mental problem typically outweigh the physical Altered Cerebral Function Therapeutic Interventions Diagnostic tests- to R/O & identify cause of altered cerebral function Medications- Isotonic IV; D50; treat narcotic overdose; fluid/electrolyte replacement; antibiotics Surgery- to remove cause Other- airway/vent; treat IICP; enteral feeding Nursing assessment specific to altered cerebral function Terms used to describe (p.1347) Description more important than term Health history- drugs/head injury/metabolic Physical exam- modify as individual cooperation Neuro Vital Signs (p.1299) Glasgow coma scale (p. 1299) Altered Cerebral Functioning: Pertinent Nursing problems Ineffective airway Risk for aspiration Risk for impaired skin integrity Impaired physical mobility Risk for imbalanced nurtition Ineffective coping- Family Home care Increased Intracranial Pressure (IICP) Normal Brain Monro-Kellie hypothesis Intracranial pressure:5-15 mmHg;60-180cm H2O Cerebral perfusion pressure: MAP-ICP=CPP; Normal: 80-100 mmHg; minimal blood flow 50; brain death 30 mmHg Autoregulation- cerebral arterioles change diameter to maintain CBF when ICP rises; need nomal range of MAP to occur; pressure (BP) and chemical (CO2) autoregulation Increased Intracranial Pressure Pathophysiology of intracranial hypertension Monro-Kellie hypothesis Cushing reflex- BP and Pulse Brain shifts- herniation syndromes Symptoms progress in relation to these physiological changes Increased Intracranial Pressure (IICP) Cerebral edema/hydrocephalus Cerebral edemaIncreases the volume of brain tissue which can cause herniation Hydrocephalus Noncommunicating Communicating Subarachnoid space with arachnoid villi Increased Intracranial Pressure (IICP) Brain Herniation Syndromes Cingulate herniation Central (transentorial) Uncal (lateral) Infratentorial herniation Extracranial herniation Brain herniation Normal brain and Herniation Syndromes Increased Intracranial Pressure Common manifestations/complications Result of compression of brain function Level of consciousness most important sign Second- pupil changes as 3rd nerve is compressed Others- p.1355 Speed of IICP how fast cause develops Cushing reflex late sign Complication of IICP is permanent disability, coma, death Increased Intracranial Pressure (IICP): Therapeutic Interventions Diagnostic tests- to find cause; monitor hydration/O2 Medications Osmotic/loop diuretics; antipyretics; anticonvulsants; antiulcer; IV fluids; TPN; vasoactive drugs for MAP; barbiturate coma Hypothermia Surgery- remove cause; shunt/drain Mechanical ventilation ICP monitoring Other monitors- Jugular venous O2; partial pressure O2 in brain tissue Intraventricular and subarachnoid monitoring devices for IICP Intraventricular drainage system Increased intracranial pressure (IICP): Nursing assessment specific to IICP Health history- assess brain involvement Physical exam Altered cerebral function assessment Frequency depends on potential IICP Early sign- change in LOC 3rd Cranial nerve compression Papilledema, projectile vomiting, vision changes, seizures (p. 1355) Late sign- Cushing VS changes– Know! Increased intracranial pressure (IICP): Pertinent Nursing Problems and Interventions Ineffective tissue perfusion: cerebral Assess/report sign IICP Adequate airway Promote venous drainage Control environment stimuli Plan nursing care Avoid Valsalva’s maneuver If bone flat out post op- assess Assess external shunts/drains